The Evolution and Impact of Point-of-care Ultrasound (POCUS) in Family Medicine: Insights from Dr. Stephen Erickson

Dr. Stephen Erickson
Transforming Family Medicine with Point-of-Care Ultrasound
The integration of point-of-care ultrasound (POCUS) has revolutionized diagnostics in family medicine, providing clinicians with real-time insights that enhance patient care (1). Dr. Stephen Erickson, a family medicine physician at Jefferson Healthcare’s Townsend Clinic in Port Townsend, Washington, has championed POCUS integration in primary care. This post explores his journey with POCUS in rural healthcare, its clinical and financial benefits, and strategies for healthcare providers to adopt this transformative technology.
Introduction to POCUS in Family Medicine
The availability of portable ultrasound machines has made it feasible for primary care physicians to conduct diagnostics typically reserved for specialists (2). With devices like handheld ultrasound and mobile ultrasound scanners, family medicine doctors can now assess musculoskeletal injuries, cardiac conditions, and lung abnormalities at the bedside (3).
For Dr. Stephen Erickson, adopting point-of-care ultrasound wasn’t just about upgrading his toolkit – it was about transforming how care is delivered in rural family medicine. “I trained 20 years ago, and even then, family doctors were learning some basic obstetric ultrasound. My interest grew alongside the industry as ultrasounds became cheaper, smaller, and easier to use,” Dr. Erickson shared.
Discover how Kosmos is making ultrasound more accessible.
Why POCUS is a Game-Changer for Family Medicine
Providing Faster, Accurate Diagnoses
Dr. Erickson emphasizes the unique advantages of POCUS in family medicine, particularly in rural settings. “I’ve always been a rural family doctor. Working in places where getting a specialist or imaging study isn’t easy made the idea of quick, reliable ultrasound appealing to me.”
He also credited the influence of emergency medicine in driving the adoption of POCUS: “The emergency department showed us how ultrasound could provide quick answers, even in austere places where other imaging isn’t easily accessible.”
Shaping Patient-Centered Care
POCUS enhances patient interactions: When a family physician can show patients what’s happening in their bodies in real-time, it changes the conversation. There’s a level of understanding and trust that develops, empowering patients to make more informed decisions about their health (4).
Expanding the Scope of Practice with POCUS
Dr. Erickson’s interest in POCUS started with a focus on obstetric ultrasound early in his career. Over time, as portable devices became more accessible, he expanded his use of ultrasound to other diagnostic applications.
“Initially, I used ultrasound to determine if a lump was a cyst or a solid mass. Then, with handheld ultrasound, I started thinking more broadly – adding lung, cardiac, and MSK imaging,” he recalled.
He emphasized the profound impact of having real-time diagnostic tools.
”It’s powerful to pivot from uncertainty to confidently deciding the next steps for a patient.”
He also suggested, ”If you want to learn point-of-care ultrasound, there are now many courses being offered that focus specifically on the needs of Primary Care doctors.”
Learn how online training can help you integrate POCUS into your practice.
Clinical Applications of Point-of-Care Ultrasound (5)
Musculoskeletal Imaging: A Game-Changer in Primary Care
Dr. Erickson shared a common scenario: “Someone comes in with shoulder pain. Instead of prescribing pain medication and sending them to physical therapy, I can immediately determine whether they need surgery or will improve with therapy.” This approach not only saves time but also ensures better outcomes.
“POCUS has also proven useful for diagnosing conditions like Baker’s cysts and rotator cuff tears. It eliminates guesswork and prevents unnecessary imaging referrals,” Dr. Erickson explained.
Cardiac and Lung Assessments: Life-Saving Interventions
He highlighted how early detection can prevent serious complications: “For heart failure patients, recognizing signs early can prevent an emergency room visit or hospital admission. It’s hard to quantify the value of what you prevent, but my hunch is this happens often when you use POCUS.”
Bladder Scanning and Urological Care
POCUS helps family physicians diagnose conditions like urinary retention and bladder stones with precision (6).
“Having tools like a bladder scanner at my disposal, which measures bladder volume automatically, means I can act immediately without relying on an external imaging center,” Dr. Erickson noted.
Obstetric Ultrasound: Improving Maternal Health
Whether it’s fetal positioning or measuring fluid levels, having the ability to scan immediately improves care for pregnant patients (7). Dr. Erickson has been performing obstetric scans for years.
He says, “Every community’s needs are unique, and as a family doctor who doesn’t practice obstetrics, you likely won’t perform as many OB scans as someone like me.”
Learn how Kosmos helps streamline diagnostic imaging for multiple applications.
The Business Case for POCUS
Cost Justification and Return on Investment
Dr. Erickson addressed one of the biggest concerns: cost. Ultrasound equipment is not inexpensive, but the ROI can become clear when a practice starts billings for scans. In one year, Dr. Erickson billed for 282 POCUS exams, generating just under $12,000 in net revenue (8).
“The powerful thing is this was just one [doctor]. And if you’re in an office with four people and you’re sharing the machine, then you’re going to recoup that four times as fast if you’re all using it. It compounds.”
Reducing Costs for Patients and Healthcare Systems
He also noted how portable ultrasound devices reduce the financial burden on patients by preventing unnecessary referrals. “For rural families, every saved trip to a hospital matters – both financially and emotionally.” Dr. Erickson said.
The EchoNous team spoke with another physician focused on this topic – read more about POCUS benefits for your practice.
Overcoming Barriers to POCUS Implementation
Training Challenges: Bridging the Knowledge Gap
Dr. Erickson stressed that learning POCUS takes commitment. It’s not just about buying the machine; it’s about learning how to use it effectively.
You need supervised practice, especially at the start. He recommended beginning with a broad skill set: “Every skill you learn makes the next one easier. Even if you don’t do certain scans often, practicing consistently builds confidence and proficiency.”
The Role of AI in Lowering the Learning Curve
“AI tools are starting to flatten the learning curve for new users,” Dr. Erickson noted. “Features that guide probe positioning or automate measurements make it easier for beginners to get good results. Every time I see a new tool at a conference, I think how much quicker I could have learned with these advancements.”
Workflow and Operational Integration
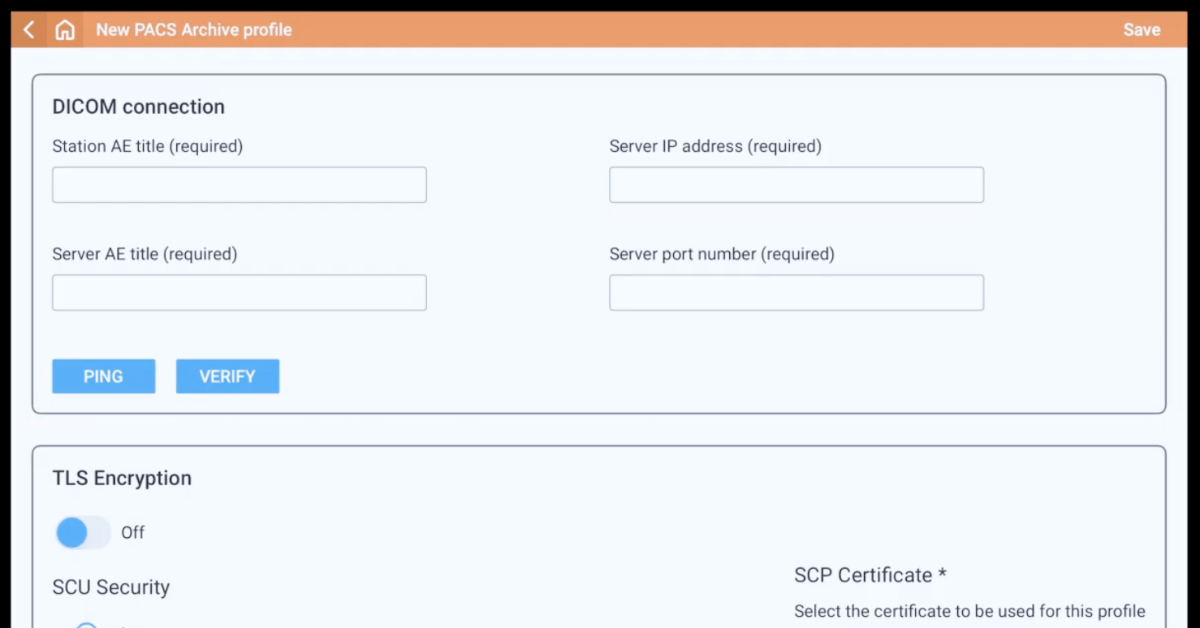
Integrating POCUS into daily practice requires careful planning. “You need a software system that archives images with patient data. Without it, meeting today’s standards for compliance and billing becomes difficult,” Dr. Erickson explained.
He encouraged collaboration with IT teams to ensure seamless integration: “The fewer clicks it takes to save and retrieve an image, the more likely clinicians are to use it routinely.”
How POCUS Improves Patient Relationships
Building Trust Through Visualization
Dr. Erickson highlighted how showing patients their scans strengthens trust: When patients can see what’s happening inside their body, they are more engaged in treatment. It demystifies the diagnosis and helps them take ownership of their health.
Reducing Anxiety with Immediate Answers
POCUS also alleviates the uncertainty that comes with delayed diagnoses. For many patients, the worst part is waiting. When a physician can give them answers right away, it eases their anxiety significantly.
The Future of POCUS in Family Medicine
AI Advancements in Ultrasound
Dr. Erickson is optimistic about the integration of AI in POCUS. AI isn’t replacing the clinician; it’s augmenting the clinician’s abilities. It gives confidence in areas where they are less experienced and speeds up the decision-making process.
Handheld Ultrasound as The New Stethoscope
He envisions a future where handheld ultrasound devices are as common as stethoscopes.
“Medical students are now emerging from their preclinical years with foundational ultrasound skills, quickly becoming adept. By the time they begin practicing, they will naturally expect ultrasound to be an integral part of their day-to-day clinical practice,” said Dr. Erickson.
Expanding Access Through Consumer Devices
Dr. Erickson pointed to emerging technologies like consumer ultrasound tools: “Imagine a heart failure patient getting an alert on their phone when B-lines appear in their lungs. That’s where we’re headed.”
Conclusion
POCUS is not just a tool—it’s a game-changer for family medicine, reshaping how clinicians approach diagnostics and patient care. By enabling real-time insights, POCUS allows family physicians to make faster, more accurate decisions, enhancing patient outcomes and overall satisfaction.
Dr. Erickson’s experiences highlight its versatility, from musculoskeletal imaging to cardiac and obstetric applications, demonstrating its ability to address various clinical needs.
Moreover, integrating AI and handheld devices like Kosmos streamlines workflows and reduces healthcare costs, making this technology a vital asset for modern practices. As adoption grows, POCUS is set to become as indispensable as the stethoscope in primary care.
Ready to embrace the future of family medicine? Learn how Kosmos can revolutionize your practice.
Citations
1. Fraleigh, C. D., et al. (2022). Point-of-care ultrasound: An emerging clinical tool to enhance physical assessment. The Nurse Practitioner, 47(8), 14.
2. Zumstein, N., et al. (2024). The use of diagnostic ultrasound by primary care physicians in Switzerland – a cross-sectional study. BMC Primary Care, 25, 246.
3. Haji-Hassan, M., et al. (2023). Efficacy of Handheld Ultrasound in Medical Education: A Comprehensive Systematic Review and Narrative Analysis. Diagnostics, 13(24), Article 24.
4. Balmuth, E. A., et al. (2024). Point-of-care ultrasound (POCUS): Assessing patient satisfaction and socioemotional benefits in the hospital setting. PLOS ONE, 19(2), e0298665.
5. Hashim, A., et al. (2021). The utility of point of care ultrasonography (POCUS). Annals of Medicine and Surgery, 71, 102982.
6. Leek, A. P. van der, et al. (2023). Point-of-care ultrasound: Usage and accuracy within a Canadian urology division. Canadian Urological Association Journal, 18(2), 48.
7. Tefera, M., et al. (2024). Health professionals’ perspectives on the role of obstetric ultrasonography in maternity care in rural eastern Ethiopia: A qualitative descriptive study. BMJ Open, 14(4), e075263.
8. Erickson, S. (2024). Financial Results of POCUS in a Family Medicine Practice: A Case Study [Poster presentation]. American Academy of Family Physicians Family Medicine Experience (FMX) Conference.