What is Point-of-Care Ultrasound (POCUS)?
The Ultimate Guide to Point of Care Ultrasound (POCUS):
Techniques, Applications, and Best Practices
POCUS Overview
What is POCUS?
Key Concepts in POCUS
Components of a POCUS System
Types of Ultrasounds Used in POCUS
Clinical applications of pocus

Emergency Medicine
In emergency medicine, POCUS plays a vital role in trauma by enabling rapid assessment using the FAST (Focused Assessment with Sonography for Trauma) protocol to detect free fluid and organ injuries. During cardiac arrest, it helps evaluate cardiac activity and volume status during CPR. It is also essential in quickly detecting and managing conditions like pulmonary edema and pneumothorax.
- Trauma: Rapid assessment using the FAST (Focused Assessment with Sonography for Trauma) protocol to detect free fluid and organ injuries.
- Cardiac Arrest: Evaluating cardiac activity and volume status during CPR.
- Pulmonary Edema and Pneumothorax: Quick detection and management guidance.
Critical Care
In critical care, POCUS is used for monitoring organ function, assessing cardiac output, renal perfusion, and other critical functions in real-time. It guides fluid management by evaluating vena cava collapsibility and performing lung ultrasound.
- Monitoring of Organ Function: Assessing cardiac output, renal perfusion, and other
critical functions in real-time. - Fluid Management: Guiding fluid therapy by evaluating vena cava collapsibility and lung ultrasound.


Primary Care
In primary care, POCUS is useful for addressing abdominal complaints by identifying gallstones, liver size, and urinary tract issues. It also helps assess musculoskeletal complaints, such as joint effusions and muscle tears, and guides injections.
- Abdominal Complaints: Identifying gallstones, liver size, and urinary tract issues.
- Musculoskeletal Complaints: Assessing joint effusions, muscle tears, and guiding
injections.
Obstetrics and Gynecology
In obstetrics and gynecology, POCUS is employed to confirm intrauterine pregnancy, assess fetal positioning, and evaluate amniotic fluid. It also assists in diagnosing gynecological issues like ovarian cysts and ectopic pregnancies.
- Pregnancy Monitoring: Confirming intrauterine pregnancy, fetal positioning, and amniotic fluid assessment.
- Gynecological Issues: Diagnosing ovarian cysts and ectopic pregnancies.

Technical Skills & Training for pocus
Basic Training
Mastering basic scanning techniques is essential for effective use of POCUS. Proper probe handling and maneuvering are crucial for optimal imaging, and identifying key anatomical landmarks ensures accurate diagnosis.
- Probe Handling: How to hold and maneuver the probe for optimal imaging.
- Anatomical Landmarks: Identifying key structures to ensure accurate diagnosis.
Advanced Techniques
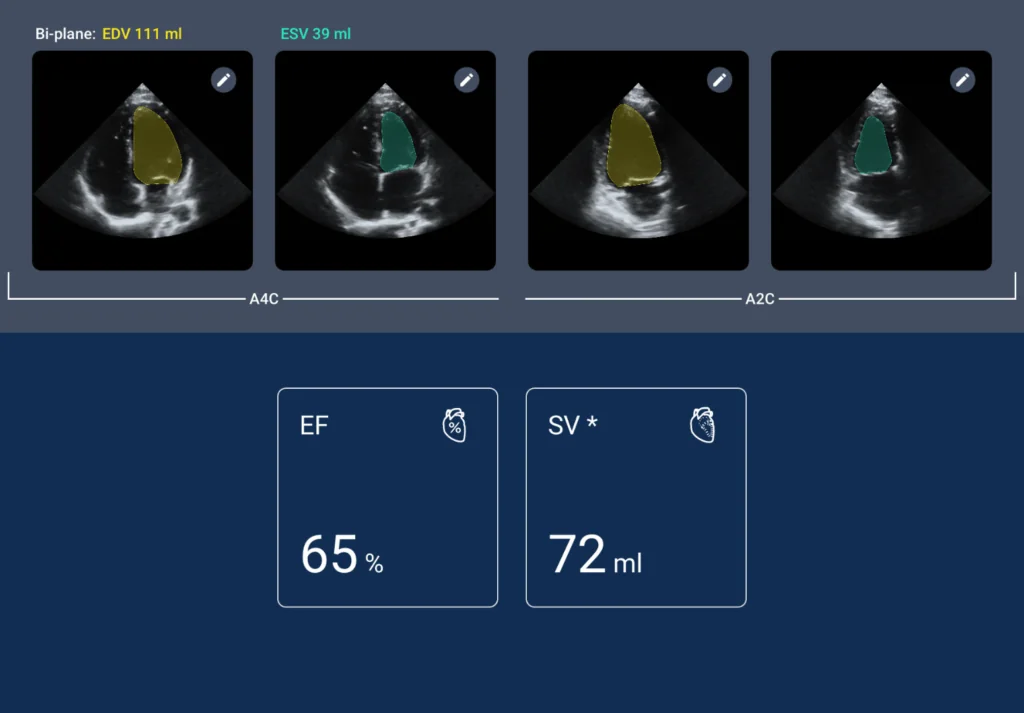
Advanced techniques include quantitative assessments, such as measuring ventricular function or fluid volumes, and using Doppler to assess blood flow in cardiac and peripheral vascular conditions.
- Quantitative Assessments: Measuring ventricular function or fluid volumes.
- Use of Doppler: Assessing blood flow in cardiac and peripheral vascular conditions.
Training and Certifications
Formal courses are recommended for training and certification in POCUS, with accredited programs offering certification. Ongoing education and skills updating are vital for maintaining proficiency in this rapidly evolving field.
- Formal Courses: Recommendations for accredited programs that offer certification.
- Continual Learning: Importance of ongoing education and skills updating.
POCUS in clinical practice
Integrating POCUS into Clinical Practice Workflow Integration
Integrating POCUS into clinical practice involves understanding when to use it. Guidelines on incorporating ultrasound examinations into routine patient assessments are important, as is proper documentation of ultrasound findings in patient records.
Decision-Making with POCUS
POCUS significantly influences clinical decision-making. Numerous examples demonstrate how it has changed patient management outcomes. However, it is essential to understand its limitations and know when to rely on more comprehensive imaging studies.
Building a POCUS Program
Building a POCUS program requires consideration of infrastructure needs, including equipment and space. Developing a training program for medical personnel is also crucial for successful integration.
challenges and limitations
Common Pitfalls
Common pitfalls in POCUS use include misinterpretation of images. To avoid these errors and improve diagnostic accuracy, continuous learning and practice are necessary. Overreliance on POCUS can be problematic; it should complement rather than replace comprehensive assessments.
Legal and Ethical Considerations
Common pitfalls in POCUS use include misinterpretation of images. To avoid these errors and improve diagnostic accuracy, continuous learning and practice are necessary. Overreliance on POCUS can be problematic; it should complement rather than replace comprehensive assessments.
future of pocus
Emerging Technologies
Emerging technologies are set to enhance the capabilities of POCUS. Artificial intelligence and machine learning are increasingly used to improve image interpretation and diagnosis. Developments in portable and wearable ultrasound technology are making it more accessible and broadening its use.
Research Trends
Research trends indicate new and unconventional applications of POCUS in medical practice. Its global impact is growing, particularly in increasing accessibility in resource-limited settings.
practical resources
Equipment Reviews
Choosing the right equipment for POCUS involves comparing features and costs of leading machines. A comparative analysis helps in making informed decisions based on practice needs and budget.
Case Studies
Case studies from various settings illustrate how POCUS has been successfully integrated into clinical practice. These real-world applications provide valuable lessons and key takeaways.
Further Reading and Resources
For further reading and resources, essential books and journals offer deeper knowledge, while online courses and workshops provide opportunities for hands-on learning.
Ready to get started?
This guide has explored the multifaceted role of Point of Care Ultrasound in modern medicine, from its basic principles to its cutting-edge applications. As technology evolves and more professionals become proficient in POCUS, its potential to enhance patient care continues to grow. Clinicians are encouraged to embrace this tool, continually educate themselves, and integrate these practices to improve outcomes across all areas of healthcare.