Exploring the Intersection of Nephrology and Point-of-Care Ultrasound, Part 2: A Conversation with Dr. Eduardo Argaiz

Dr. Eduardo Argaiz
MD, PhD

Luke Baldwin
VP of Global Marketing, EchoNous
This is the second half of our interview between Luke Baldwin, VP of Global Marketing at EchoNous, and Dr. Eduardo Argaiz, MD, PhD, who is expanding the boundaries of Point-of-Care ultrasound (POCUS) in nephrology.
If you haven’t read part one, where Dr. Argaiz shares details of his own journey into POCUS, you can do so here.
[Note: This interview has been edited for clarity and brevity.]
Getting Started with POCUS: Certification, Training, and Equipment
Luke Baldwin: So, let’s say you’ve convinced a nephrologist of the benefits, and they’re eager to enhance their practice with ultrasound. How do they begin if they’re new to ultrasound?
Eduardo Argaiz, MD: That’s a great question. Certification is key, and it varies by country. In the US and Canada, nephrologists should focus on available CME courses that different organizations offer.
For example, the American Society of Diagnostic and Interventional Nephrology (ASDIN) regularly offers ultrasound CME courses. After completing a few courses, you can apply for certification by submitting your supervised scans for evaluation. This certification program provides a pathway for proficiency in point-of-care ultrasound, a valuable skill in nephrology practice.
We’ll have our annual meeting on February 24th (2024) in New Orleans, where we’ll teach point-of-care ultrasound, covering basic and advanced topics. This is an opportunity for nephrologists to gain expertise without committing to extensive training periods. They can pursue this training alongside their practice or afterward.
Another option is to explore workshops that mainstream nephrology associations offer during their annual meetings. For instance, the National Kidney Foundation will host a workshop in California in May this year. The American Society of Nephrology will also hold a POCUS workshop in California, where I’ll be teaching. Local workshops, like the one by the National Kidney Foundation of Arizona in March 2024, also provide valuable learning opportunities.
To start your POCUS journey, find the annual workshop nearest to you. Then, dedicate yourself to accumulating studies, saving images, and seeking certification from organizations like ASDIN to validate your expertise.
Luke Baldwin: So, they’ve got a pathway to certification now. They’re on board with the idea, but now comes the question of what kind of ultrasound technology they need. What factors should they consider when choosing an ultrasound product? Should they simply opt for the cheapest option, or is it better to invest in something more advanced right from the start? How do you advise people in selecting equipment?
Eduardo Argaiz, MD: Some might think it’s logical to go for the cheapest option while still learning, but that’s a mistake. A high-quality machine is crucial for obtaining clear sonographic views and good-quality images, especially for novices. A less powerful machine can significantly prolong the learning curve because obtaining images can be more challenging.
I recommend aiming for a slightly more high-end ultrasound machine. If you’re already investing, why settle for a machine that lacks the capabilities you may need as you progress in your expertise, particularly in product and hemodynamic assessment?
Even if you’re unfamiliar with advanced features like pulse wave Doppler or tissue Doppler imaging, investing in a high-end machine is beneficial. It ensures better image quality and prepares you for potential advancements in your skills. Hemodynamic assessment for nephrologists extends beyond basic 2D heart imaging; it includes measurements such as cardiac output, filling pressures, diastolic abnormalities, and pulmonary systolic pressures, for which you need continuous wave Doppler, and venous congestion, which is coming here to change the game.
Consider your work setting when choosing the machine. Cart-based ultrasound machines may be more convenient in an intensive care unit, whereas portable machines are preferable in ambulatory clinical settings or when moving between hospitals. Portables are also useful when machines are in high demand, such as during procedures like central line placements, where having your own machine can save time.
Ultimately, investing in a high-quality ultrasound machine tailored to your work environment and potential future needs is the wisest choice for those entering the field.
Advanced Applications of POCUS: Beyond Basic Imaging
Luke Baldwin: What was your first exposure to our Kosmos products? I understand you’re a big fan. When did you first learn about it, and what about the Kosmos system stood out to you?
Eduardo Argaiz, MD: I think it was also from Philippe. By then, I was already a geek, particularly fascinated with assessing venous congestion using Doppler ultrasound. But, at the time, none of the portable ultrasound machines available allowed me to do this at a high-end level, which was a fundamental limitation. Some of my friends had purchased some of the commercial portable ultrasounds, and I tried them out, but I couldn’t get the portal vein Doppler or intrarenal venous Doppler, which is the hardest.
Then, my friend Philippe showed me this portable machine [Kosmos] and looked at the Doppler tracings, and I was hooked. I said, “I need to get my hands on one of these.” It’s always good to get a recommendation from a friend and cut straight to what works.
Luke Baldwin: Considering where your passion lies, understanding beyond just what’s happening with the kidney but also with the heart and hemodynamic assessment, what value does the Kosmos system have in clinical applications for a comprehensive diagnosis in nephrology?
Certainly, we have Doppler, pulsed wave, and continuous wave capabilities, as well as cardiac capabilities. So, what value does Kosmos offer in providing a broader, more comprehensive view than what’s typically available?
Eduardo Argaiz, MD: Many aspects of the Kosmos machine have helped us tremendously in our clinical practice. The main areas for nephrology would be hepatorenal syndrome and cardiorenal syndromes, where you need a detailed hemodynamic assessment to tackle these diseases.
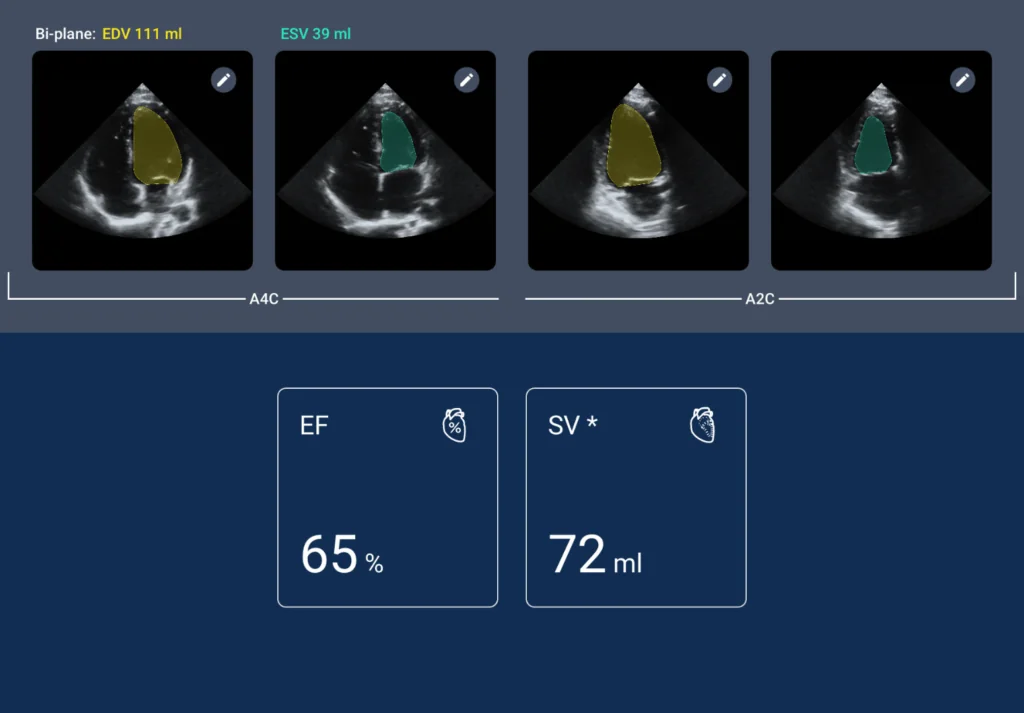
One of its most beautiful aspects is the artificial intelligence measurement of ejection fraction.
Sometimes, I would ask a resident or fellow to perform a point-of-care ultrasound. I would trust their images and ejection fraction assessment because they show me the data [gathered] from artificial intelligence. Also, it takes way less time than actually doing Simpson’s biplane method.
I like that for assessment of just the systolic function of the left ventricle; this always changes management.
I frequently use this in our patients with cirrhosis and acute kidney injuries. It’s very different from having a patient with cirrhosis and a left ventricular ejection fraction of 15 than the usual patient with hyperdynamic circulation and a left ventricular ejection fraction of 70, which would benefit from radically different treatments, and you know Kosmos delivers that information in a couple of seconds, so I like that.
A little bit more the advanced applications, I would say the pulsed wave Doppler is excellent; it allows me to measure cardiac output and, of course, Venous congestion, and you know I’ve come to appreciate the ability to have the continuous wave Doppler because many of our cardiorenal patients, especially at my shop, is a place that specializes in autoimmune disease so we have a lot of pulmonary hypertension or primary pulmonary hypertension.
Being able to assess pulmonary filling and arterial pressures, which can only be done by continuous wave Doppler, you know, really helps me phenotype the type of venous congestion I’m looking at.
One of the most relevant applications of continuous wave Doppler in critical care nephrology is assessing obstruction of the left ventricular outflow tract. So, measuring the velocities of blood flow in the left ventricular outflow tract, when there is obstruction, velocities will go from the usual 1-centimeter per second to more than, you know, 4 or even 5 centimeters per second, and this can only be assessed with continuous wave Doppler. This diagnosis of left ventricular flow tract obstruction changes management radically, and it might mean life or death if you don’t make this diagnosis in time. So, you know, we see this all the time in our patients with cirrhosis. Maybe a lot of patients with sepsis and acute kidney injury also present with this condition, and this can only really be assessed with a high-end, high-value point-of-care ultrasound machine.
Luke Baldwin: Very interesting. While I’m not a physician who would use this technology to save patients’ lives, understanding where continuous wave Doppler, in particular, can be helpful and in what situations having that tool available matters is crucial. Otherwise, what alternatives would there be?
Eduardo Argaiz, MD: Yeah, there is no way without CW. You would get a pulse wave, which would suggest it’s higher than 200 centimeters or 2 meters per second, but a pulse wave doesn’t go higher. So, you would be left guessing without it.
Luke Baldwin: Yeah, you’d either guess or have to find another ultrasound system.
Eduardo Argaiz, MD: I mean, for example, for pulmonary artery pressures, you would need to put as a catheter, like a pulmonary artery catheter, which is an invasive technique, but for left ventricular tract obstruction, there’s no substitute for CW. Not even invasive hemodynamic measurements can diagnose this condition so you’re left without the diagnosis if you don’t have the CW.
Luke Baldwin: OK, interesting, so the decision you make could go one way or the other.
Eduardo Argaiz, MD: Yes, it can significantly alter outcomes. This is one of the few conditions where it’s fundamental to have this diagnosis because, in a matter of minutes or hours, the patient might crash if you don’t diagnose it in time.
Educational Initiatives and Promoting POCUS in Latin America
Luke Baldwin: Do you have any other topics you wish to discuss or any new research you would like to share with our audience? What’s on your mind that you would like to highlight?
Eduardo Argaiz, MD: I want to highlight the Latin American Society of Nephrology and Hypertension (SLANH). This is our largest Latin American nephrology association, and it’s working together with the International Society of Nephrology (ISN) and our group at the Argentinian Society of Critical Care Ultrasound (ASARUC).
Together with these three organizations, we plan to reach as many nephrologists as possible to get them a complete education on point-of-care ultrasound, covering the interventional aspects of point-of-care ultrasound and the diagnostic and hemodynamic assessment aspects.
We are conducting our extensive workshop in Colombia; this will be in June 2024. We are preparing an outstanding curriculum for online theoretical classes and courses. You can take it before or after the workshops. This will be the first point-of-care ultrasound workshop sponsored by the Latin American Society of Nephrology and Hypertension, but it won’t be the last. So, keep an eye out for more workshops and more courses that we’re going to offer both online and in several countries in Latin America.
Colombia is just the first one, but this will be big, and really, the efforts of the Latin American Society of Nephrology are unparalleled. I have yet to see any other society so interested in teaching point-of-care ultrasound in so many countries in, you know, so many remote areas. I hope this increases the usage and application of point-of-care ultrasound for all nephrologists.
Luke Baldwin: That’s exciting! So, Colombia, 2024?
Eduardo Argaiz, MD: Yes, Colombia, June 2024. It’s going to be for 100 students, so it’s going to be significant.
Luke Baldwin: That sounds fantastic. Thank you for sharing that information. Thank you so much for joining us; it was great to meet you.
Eduardo Argaiz, MD: Thank you for having me.
To learn more about Kosmos, contact us today!