How AI Can Make Diagnoses Faster and Easier:
A Conversation with Dr. Benjamin Hibbert

Dr. Benjamin Hibbert, MD, PhD
Interventional Cardiologist and
Critical Care Specialist

Luke Baldwin
VP of Global Marketing, EchoNous
Luke Baldwin, VP of Global Marketing at EchoNous, recently sat down with Dr. Benjamin Hibbert, whose work explores the ways that AI can make ultrasound technology more accessible for all patients. In this conversation, Baldwin and Dr. Hibbert discuss the role that ultrasound can play in reaching underserved patients and improving the assessment process.
[Note: This interview has been edited for clarity and brevity.]
Introduction
Dr. Benjamin Hibbert is an interventional cardiologist and critical care specialist at the Mayo Clinic in Rochester, MN. His extensive expertise centers on managing structural heart disease, including procedures such as stenting and valve repairs.
Early Exploration of Ultrasound
Luke Baldwin: After working so hard to create a product that closes real-world healthcare gaps, it is always thrilling to hear about how the Kosmos system is making an impact. To get started, can you tell us about yourself and your background with POCUS?
Benjamin Hibbert, MD: I do interventional cardiology, specifically structural heart disease. I spend my days stenting and fixing valves. But, I also do my ward work as a critical care cardiologist. As a critical care cardiologist, I work in the cardiac intensive care unit (ICU). Cardiac ICU is where the sickest cardiac patients go and we use POCUS multiple times per day to evaluate and monitor patients.
I’ve been doing research on POCUS for approximately 10 years in various academic research positions in Ottawa, Canada. I had been using POCUS routinely as part of my clinical practice. Currently, I am continuing my work at the Mayo Clinic.
Luke Baldwin: Can you describe your latest article and research study? How did the Kosmos tool perform?
Benjamin Hibbert, MD: We wanted to analyze how the AI-assisted POCUS (Kosmos system) performed by a novice user compared to the gold standard cart-based ECHO (echocardiography) performed by experienced sonographers in optimal conditions. As you know, optimal conditions are not realistic in real-world situations. In fact, the optimal conditions necessary for cart-based ECHO make it extremely expensive as well as difficult to schedule and obtain.
During the study, the AI integrated into POCUS produced diagnostic-quality images matching an ECHO in optimal conditions. What we also found is that the AI POCUS also worked well in real-world conditions. As we know, most real-world POCUS is performed in sub-optimal conditions with inexperienced or novice-level users. Our study found that AI POCUS done with a novice user produced equal diagnostic quality images to cart-based ECHO for accurate patient treatment.
One advantage of POCUS is its portability. POCUS can be used to reach patients in a larger variety of environments. We were impressed with how the POCUS performed in real-world conditions.
Luke Baldwin: What are the implications of your findings?
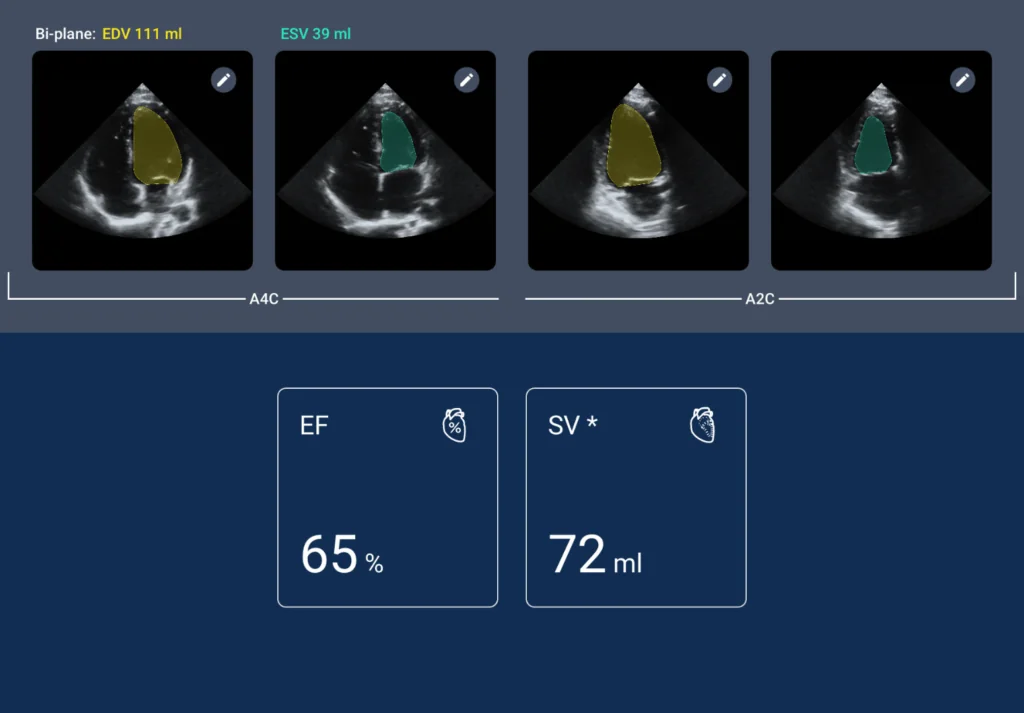
Benjamin Hibbert, MD: Our findings suggest that POCUS can be used instead of a full ECHO for patient condition monitoring and when only a specific diagnostic test is required. For example, instead of always having to order a full ECHO for a single ejection fraction test and then wait for the results for a dozen images, I can use the POCUS and get only diagnostic images for ejection fraction.
POCUS has advantages in portability and ease of use. It can also significantly reduce the cost of healthcare when a full ECHO is not necessary.
POCUS enables the democratization of healthcare screening to improve patient access. Many patients currently go unscreened for heart conditions until they experience a health event like cardiac arrest. Many patients don’t have access to quality healthcare or screening. The integration of AI in POCUS allows us to perform more outreach. Access to easy, high-quality diagnostic screening that provides immediate results and works within the existing clinical workflow is crucial to improving cardiac patient care.
POCUS is democratizing access to effective and efficient screening. It can be used nearly anywhere and provides diagnostic quality scans even when used by novice users. Additionally, the AI assistance features are useful for accurate image interpretation. Family physicians and retail health clinics can effectively scan patients to better detect early signs of heart disease. In reality, POCUS extends a healthcare provider’s reach.
Diagnostic Accuracy and an AI Safety Net
Luke Baldwin: Were there other findings within your research that were surprising to you?
Benjamin Hibbert, MD: Yes, we were surprised at how well the tool provided high-quality diagnostic images in real time. I’m not surprised that our expert sonographers were able to get quality images, but we were impressed that the novice and less experienced users were also able to generate high-quality images. When we can get high-quality diagnostic images in any clinical setting, it allows for more accurate diagnosis and treatment.
AI tools like Kosmos provide a safety net for any user. For example, AI assistance tools for getting the right image are helpful for training and diagnostic accuracy. Now you have two major uses for AI in POCUS: training and accurate diagnosis.
Everyone needs to see the potential application of AI in medical technology. The number one reason ECHOs are done is to assess for left ventricular ejection fraction. It’s the type of measurement that lends itself nicely to AI-based technology. The fact that AI is built into the POCUS technology means you get the results in real time. Results in real time means the physician can do a bit of quality control and review results immediately. Additionally, I’m not having to move out of my normal clinical workflow. For example, I’m not having to upload images and wait for them. I get the answers I need immediately.
It gives me confidence that when people are out there using this device, they’re sending back the diagnostic quality necessary for medical providers to make accurate clinical decisions.
Reducing Costs While Improving Patient Outcomes
Luke Baldwin: I’m sure you have, or know of, patients that are in the late stages of cardiac disease. When they finally get screened, it is nearly past the point of treatment. When you can diagnose cardiac issues earlier, doesn’t it improve patient outcomes?
Benjamin Hibbert, MD: I think we can answer most clinical questions with a POCUS. The problem is many patients don’t have access to screening until they are in the ICU. In practice, I can use the POCUS technology to perform the initial screening to see if a full ECHO is necessary. If I can quickly image the ejection fraction, then I have an answer without getting 100 images from a full ECHO.
POCUS tools provide access for patient screening and monitoring, especially in real-world situations where patients cannot easily get follow-up testing. With POCUS, follow-up and patient monitoring can be done at the point of care. Even if the user has little experience, you have confidence that the image quality is high as is the initial interpretation of results.
For example, we can use POCUS and build screening programs nearly anywhere, such as if I as a patient get a screening for cardiac disease at Walmart and discover an issue. My medical provider then has a chance to refer me to a specialist or begin treatment before it ends in an emergency or death. When we can identify cardiac disease earlier, then it bends the needle on the patient’s prognosis and long-term quality of life.
ECHO is costly, so once payers catch up with the fact that POCUS screening is more cost-effective for determining ejection fraction, for example, then it saves them and the patient money. Cardiac screening may become as common and as cost-effective as a routine blood pressure test. It’ll reduce the number of emergencies that incur much higher healthcare costs
Future of AI in the Treatment of Heart Disease
Luke Baldwin: In the future, do you see the Kosmos tool and its flavor of AI being especially helpful compared to other AI models?
Benjamin Hibbert, MD: The answer is I don’t know. It’ll be up to companies like yours that develop medical AI solutions. Any new AI models will need to be validated within the healthcare system to verify they perform the function with the accuracy and quality necessary. Any AI tool must be integrated into the clinical workflow. POCUS doesn’t require any extra steps and we get the quality data we need in real time. Any other tools must be integrated into the clinical care workflow.
The future of POCUS with AI as a screening and exam tool is exciting. We can use it to create screening programs in underserved populations around the globe. We can use POCUS with AI to make cardiac screening similar to a colonoscopy. At a certain age, everyone gets a cardiac screening. We can prevent patient emergencies by expanding screening access with POCUS. Additionally, we can provide patient monitoring solutions when a full ECHO is not feasible.
POCUS could expand and provide screening for other heart conditions. You know valvular heart conditions are reaching epidemic levels. If we can easily and cost-effectively reach more patients with POCUS, we can treat more patients sooner with positive results. POCUS cardiac screening could even become part of a normal medical screening performed at any doctor’s office or clinic.
To see the AI capabilities Dr. Hibbert’s team used in their study, click here.