From Rural Reality to Revolutionary Research: The Inspiring Journey of Dr. Diana Foo

Dr. Diana Foo
“The worst nightmare is having a very acutely ill patient…knocking at your door at 12 midnight”. For Dr. Diana Foo, this wasn’t a hypothetical scenario; it was the reality of being a new medical doctor in a resource-constrained rural hospital in Malaysia. She recalls the immense challenge of transferring patients, a journey of at least three hours that required crossing two ferries. In emergencies, it meant using small speedboats with no medical equipment, in pitch-black conditions.
These formative experiences, witnessing the consequences of delayed care, shaped her passion to bridge the gap between well-equipped tertiary hospitals and community-based primary care. This is the story of how one doctor’s vision, developed from her experiences with real-world challenges, is now impacting cardiac care.
A Path Forged by Necessity
Dr. Foo’s journey in medicine was shaped by her time serving in rural communities. The challenges she faced sparked a strong interest in early prevention and detection. This drive led her down an unconventional path in Malaysia’s medical system. Instead of pursuing a traditional specialization first, she dove into clinical research, a field for which there was no established career pathway for academic specialists within the Ministry of Health. It was a journey that required personal sacrifice and faith in herself and her community.
Later, recognizing the need for management and negotiation skills to lead complex, multidisciplinary projects, she pursued an MBA—another non-traditional step for a clinician. Her motivation remains clear: “To do clinical research, we stay closer to patients,” a belief that has kept her working within the Ministry of Health, where the largest patient populations are managed.
The Heart2Miss Initiative: A New Model for Cardiac Care
Dr. Foo’s experiences contributed to the creation of the “Heart2Miss” initiative, a project designed to detect heart failure early in diabetic patients. The name itself is a double entendre, signifying the mission to “not miss heart failure” while rhyming with “hard to miss”. The project tackles a core problem she witnessed years ago: the bottleneck of diagnostics in centralized, tertiary hospitals.
The traditional path to diagnosis involves long wait times—sometimes six months to a year—for an echocardiogram at a public tertiary hospital. To overcome this, Dr. Foo’s team developed a decentralized repeat echo triage model. This “hub-and-spoke” system acts as a filter, ensuring that specialized care is directed to those who need it most.
Here’s how the model works:
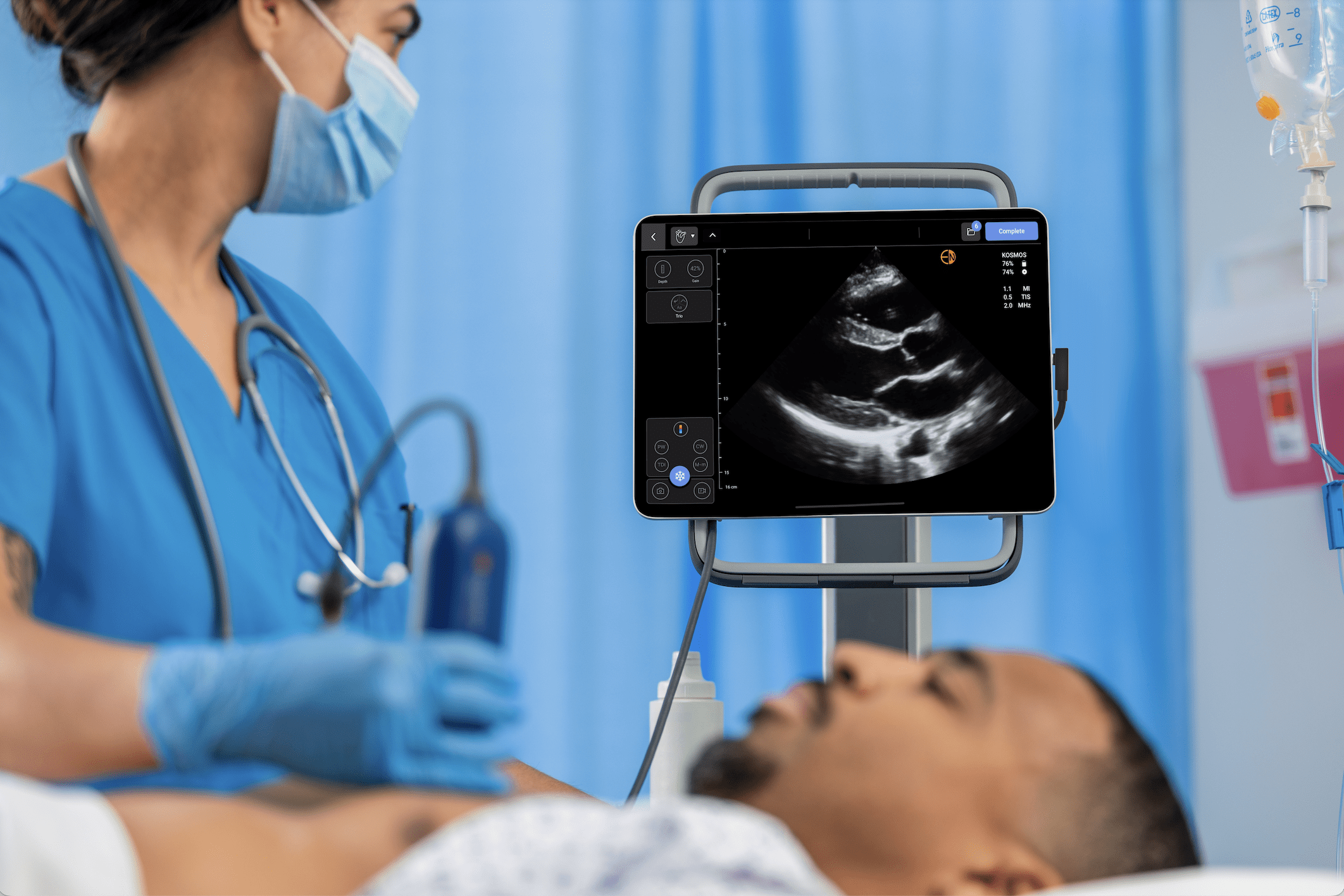
The Spokes (Primary Care): The process begins in local primary care clinics. Here, a novel workforce of trained bioscience graduates—a group often underemployed in Malaysia—act as mobile community sonographers. In collaboration with US2.AI, a structured four-week training program was designed specifically for these novices who had no prior medical training. The program consisted of three weeks of theory and one week of intensive hands-on practice. The training taught the graduates how to perform a rapid, three-view cardiac scan (parasternal long-axis, apical 4-chamber, and apical 2-chamber) using the portable, AI-powered Kosmos ultrasound system. A key part of the training involved teaching them to understand the images they were capturing, using layperson language—for example, instructors would tell them to “fan it up” or “fan it down” instead of using more clinical terms like “angulate,” which helped the novices understand probe motion. This approach equipped them to conduct the initial screenings effectively and explain the basics to patients when asked.
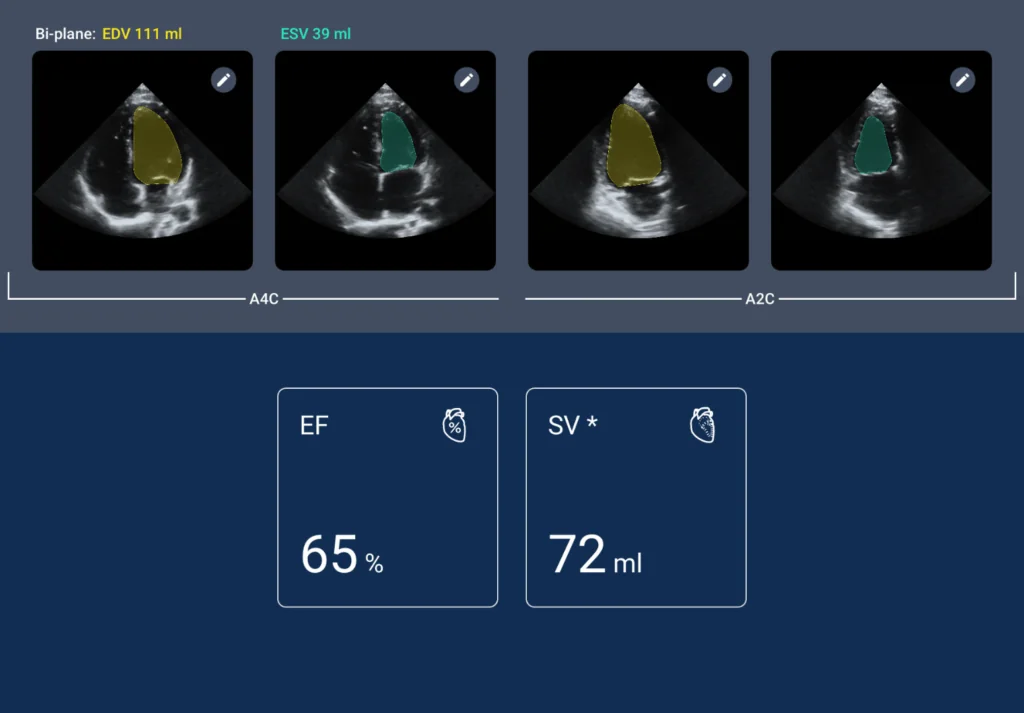
The Intermediary (The Core Lab): The images and AI-driven measurements are sent to a central core lab. Here, experienced sonographers remotely verify the results of the initial scan. This intermediary step is the model’s filter. The results demonstrated the model’s efficiency: 77.3% of the 985 patients screened were found to have normal echoes and were excluded from needing further scans. Patients with abnormal or incomplete scans (22.7%) at spokes primary care trigger a second, full confirmation scan at the intermediary (core lab). This immediately removes the majority of cases from the queue, freeing up system resources.
The Hub (The Tertiary Center): Ultimately, only 1% of the entire patient group screened needed to be referred to the “hub,” or the heart failure specialist at the tertiary center, for diagnosis and intervention.
This model effectively offloads the diagnostic and referral burden from specialist centers while providing essential support to primary care physicians, allowing them to intervene earlier with readily available medications
The Role of AI and a New Workforce
This decentralized model is enabled by technology and a new approach to the workforce. The Kosmos system by EchoNous, with its integrated AI and Us2.ai software, was a key enabler.
The AI provides real-time guidance on probe positioning and image quality, which allowed Dr. Foo’s team to train complete novices in just four weeks—a process that traditionally takes at least six months for a full examination. These newly trained sonographers were able to screen up to 30 patients per day, a rate difficult to achieve with manual systems. Their performance improved with experience, with scan times decreasing and analyzable image acquisition rates exceeding 85% after four weeks of training.
This initiative does more than just detect disease; it creates opportunity. By training and employing bioscience graduates, Dr. Foo is building a new, sustainable diagnostic workforce, providing STEM-aligned career opportunities while solving a healthcare shortage.
The Road Ahead
Dr. Foo hopes to scale the Heart2Miss initiative and is eager to share the model with other resource-constrained regions globally. The path to wider implementation involves overcoming challenges, including formally integrating this new workforce into the healthcare system and gaining policy support by demonstrating the long-term cost savings of early prevention.
Her journey—from a doctor in a small rural hospital to a leader in health innovation—demonstrates that difficult challenges can inspire effective solutions. By re-examining the status quo, Dr. Diana Foo is not just changing the outlook for heart failure patients; she is contributing to the future of healthcare delivery.