Identifying & Diagnosing Aortic Stenosis
Patient: An 82 year old female patient presented to the ER with symptoms and signs of congestive heart failure.
Initial Examination: She had a history of well controlled hypertension treated with beta blockers and diuretics by her primary care physician. On cardiac auscultation a mid-systolic ejection murmur was noted with diminished S2 heart sound. Her jugular veins were dilated and mild lower limb edema was present.
Kosmos POCUS Examination: Bedside examination with KOSMOS revealed severely impaired left ventricular systolic function. The aortic valve was heavily calcified and had severe stenosis. Moderate functional mitral regurgitation was also present. Patient was treated with intravenous diuresis resulting in improvement of her symptoms. A subsequent coronary angiogram revealed no coronary stenoses. She was scheduled for a TAVI procedure.
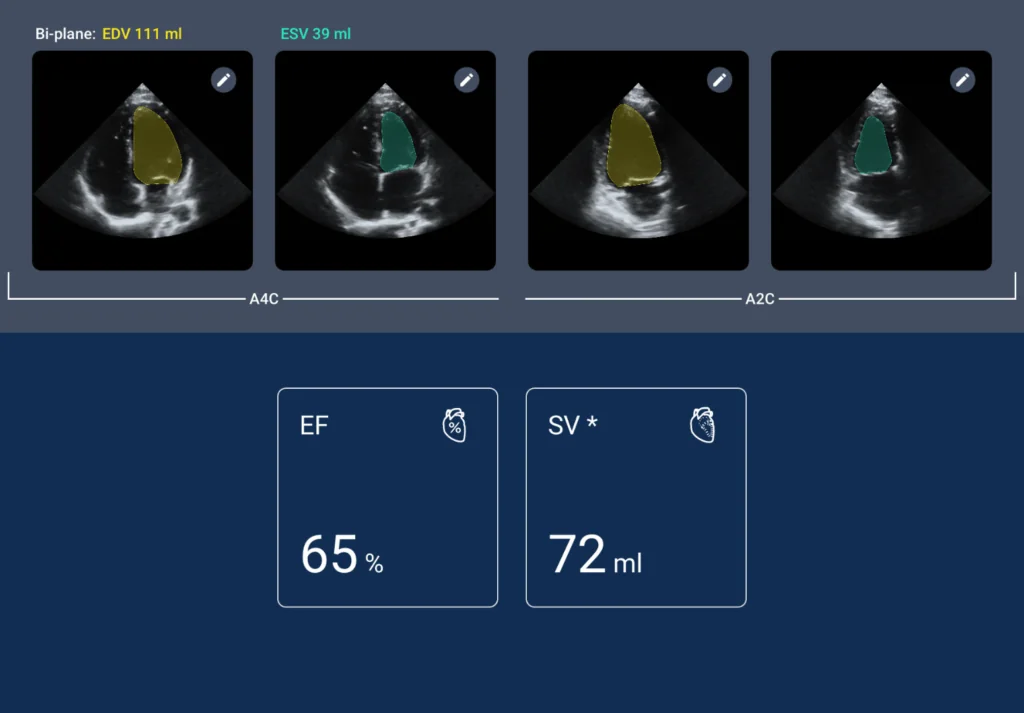
Figure 1
Automated EF calculation with KOSMOS AI confirming the visual impression of severely impaired LV systolic function.
Video 10
A4C view with color showing moderate functional mitral regurgitation.
Video 11
CW MR signal from apical four chamber view.
Video 12
A5C view with color showing turbulent flow through the stenosed AV.
Video 13
CW AS signal from A5C view.
Figure 2
Maximum aortic valve velocity measured at 3,7-3,8 m/s with CW.
Video 14
CW AR signal from A5C view.
Video 15
PW LVOT signal showing reduced forward LV stroke volume
Figure 3
Maximum LVOT velocity measured at 0.54 m/s with PW, suggestive of low flow state.
Video 16
A4C view with color showing mild functional tricuspid regurgitation. There is also color flow inside the RA coming from the IAS, suggestive of a patent PFO with left to right shunt due to increased LA pressure.
Video 17
Subcostal view showing dilated IVC.