The Rationale for Ultrasound-Guided IV Access
Why use ultrasound for IV access?
Placing a peripheral intravenous (PIV) catheter is a basic skill in healthcare. Millions of these procedures happen each year in various clinical settings. However, for a significant number of patients, achieving IV access is anything but routine. As many as 30% of adults and 50% of children are estimated to have difficult venous access (DVA). This can lead to multiple attempts at cannulation or the need for a central line. An estimated 35 to 50% of PIV cannulation attempts fail, which can result in complications, both immediate and delayed.

Table of Contents
- The Rationale for Ultrasound-Guided IV Access
- Why use ultrasound for IV access?
- Clinical guidelines supporting ultrasound-guided IV placement
- Evidence on first-pass success and improved patient outcomes
- The role of ultrasound in reducing central line utilization
- Clinical use access and special populations
- Looking ahead: next steps
- Letʼs talk about implementation
- FAQs
- References
Ultrasound-guided peripheral IV (USGPIV) access offers a transformative solution. Real-time imaging allows clinicians to see target veins. They can then guide needle placement with precision. This leads to quicker and more successful cannulations, especially in difficult cases. This article reviews the reasons for using USGPIV. It highlights key guidelines and growing evidence about the effects on patient outcomes and central line usage.
Clinical guidelines supporting ultrasound-guided IV placement
Ultrasound for vascular access has evolved from a technique reserved for specialists to the standard of care endorsed by leading healthcare organizations. Clinical guidelines increasingly recognize ultrasound as an adjunct for complex cases and a proactive solution for improving safety, efficiency, and outcomes across patient populations.
- In 2021, the Infusion Nurses Society (INS) updated the 8th edition of Infusion Therapy Standards of Practice to recommend ultrasound guidance for patients with DVA, including those who have failed traditional attempts. The INS emphasizes the importance of trained personnel and image-guided insertion to improve outcomes [1].
- The American College of Emergency Physicians (ACEP) encourages using point-of-care ultrasound (POCUS) for PIV access, particularly in emergency and trauma settings where rapid, reliable vascular access is critical.
- The Agency for Healthcare Research and Quality (AHRQ) includes ultrasound-guided vascular access in its recommended patient safety practices, citing the role of USGIVA in reducing complications and preventing escalation to central venous access.
- The American Institute of Ultrasound in Medicine (AIUM) promotes ultrasound as a core tool in vascular access protocols and supports competency-based training for clinicians.
These guidelines reflect a shift toward outcome-focused care, where real-time visualization is no longer considered optional but essential for high-quality IV access. [2,3,1]
Evidence on first-pass success and improved patient outcomes
The most compelling case for ultrasound guidance lies in the numbers. Research shows that USGPIV boosts first-attempt success rates. This is especially true for patients with hard-to-find veins. It also reduces the time, discomfort, and uncertainty of blind attempts.
Key Evidence:
- A meta-analysis in the Journal of Vascular Access revealed that USGPVA. Ultrasound guidance improved success rates when compared with traditional techniques [pooled odds ratio (OR) 3.96; 95% confidence interval (95% CI) 1.75-8.94] [4].
- Another meta-analysis by Tran et al. in Ultrasound in Medicine & Biology showed a twice higher likelihood of first-attempt success with USGPVA, significantly fewer attempts at cannulation, and higher patient satisfaction [5].
Pediatric studies have echoed these findings, with ultrasound leading to faster access and significantly fewer needle sticks in children, who often have smaller and less visible veins. One study of pediatric ED patients with difficult venous access compared the success rate of an intravascular (IV) access procedure at the first attempt, with and without ultrasound assistance.. The results of this study showed the success rate at first attempt with ultrasound at 90% vs. 18% in the group randomized to traditional cannulation [6].
Additional Outcomes:
Lower complication rates:
Complications arising from frequent insertion attempts and suboptimal placement of PIVCs encompass an elevated risk of phlebitis, thrombosis, and catheter-related infections, heightening the likelihood of early device failure. The failure rate of PIVC ranges from 35% to 50%. Subsequent PIVC failures are more likely after an initial PIVC failure [7].
By enabling accurate vessel selection and real-time needle guidance, ultrasound reduces the likelihood of hematomas, arterial punctures, and catheter dislodgement.
Improved catheter longevity:
Proper placement in larger, deeper veins contributes to longer-lasting access and reduced need for reinsertion [8].
Enhanced patient satisfaction:
Avoiding multiple failed attempts and minimizing discomfort translates directly into higher patient-reported satisfaction and better Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores [9].
These results support using ultrasound for problem-solving and as a first-line strategy to optimize vascular access on the first try.
The role of ultrasound in reducing central line utilization
One of the most significant benefits of USGPIV is its ability to reduce unnecessary escalation from peripheral IV access to a central venous catheter (CVC) placement. Central lines, while effective, come with a well-documented risk profile, including bloodstream infections, deep vein thrombosis, and higher procedure-related costs.
The average cost of placing and managing a central line ranges from $2,000 to $5,000, not including treatment costs for complications. The CDC estimated the cost of a central line infection to be $46,000 in 2016; other studies have estimated average costs to be $17,896–$94,879. Hospitals can save hundreds of thousands of dollars annually by preventing even a small number of CVC placements [10].
Advantages of USGIVA
Key advantages of USGIVA include the following outcomes:
- Prevention of escalation:
- When clinicians can obtain reliable peripheral access using ultrasound, they avoid escalating to PICCs, midline catheters, or central lines— especially in non-critical patients.
- Lower infection risk:
- Central line-associated bloodstream infections (CLABSIs) are a major safety concern. Each avoided central line represents a win for patient safety and quality metrics [11].
- Lower risk of complications associated with multiple cannulation attempts [12,7]:
- The prevalence of PIVC failure ranges from 35% to 50%. The risk of failure of each subsequent PIVC is elevated following PIVC failure.
- Cost savings:
- A recent observational cohort study at a tertiary academic center found that when healthcare professionals who had undergone ultrasound training for vascular access were compared to placement of PIV by professionals with traditional training in PIV cannulation (Operation Stick), the incremental cost (ΔC) for each patient in the USGPVA group was -$83.175 (95% CI: -$103.953 to -$62.398; p<0.001), indicating that the ultrasound group saved money compared to the non-ultrasound group [13].
Some illustrative cases:
- A study of a nurse-led training course for RNs on USGIVA resulted in a successful first-stick cannulation 83% of the time in proctored cannulations. The study concluded that a successful nurse training program could be developed at a lower cost than the associated costs of one central line infection [14].
- A 5-year study during the implementation of an ultrasound program in a large urban ED found that the number of patients who required central line placement dropped by 80% over the five years. The proportion of central lines placed in critically ill patients increased from 34% to 81% because of the drop in central line placement in non-critically ill patients [15].
- A study that examined the use of USGIVA in pediatric patients found that first-stick attempts were successful 80% of the time with ultrasound guidance, compared to 64% of successful initial attempts using traditional methods. The same study showed decreased time required with ultrasound, which averaged 6.3 minutes compared to 14.4 minutes with traditional methods. In addition, the median number of attempts was 1 with ultrasound and 3 with conventional attempts [6].
Clinical use access and special populations
Ultrasound-guided IV access is not limited to emergency medicine or intensive care. It has expanded applications across various departments and patient populations, especially as handheld and cart-based ultrasound systems become more accessible.
Key Use Cases:
- Although ultrasound-guided IV access has been widely adopted, it is often prioritized in those patients with difficult venous access. These patients include those with a history of IV drug use, patients on hemodialysis or with current hypotension, dehydration, edema, coagulopathy, chemoradiation, and obesity [16].
Emergency departments:
Of approximately 100 million annual patient visits to the emergency department, nearly 60% require a PIV, with 90% of admitted patients requiring one. Rapid access is critical in many cases, and delays can be life-threatening. USGPVA has been shown to decrease the number of attempts and length of time to cannulation.
In each case, ultrasound reduces provider frustration, patient stress, and resource utilization across departments. It helps stabilize patients faster and reduces crowding.
Oncology and hematology:
Many cancer patients have fragile veins and long treatment histories. Preserving venous access with well-placed peripheral lines is critical.
Obese and bariatric patients:
It can be difficult to find a vein when much adipose tissue is present. Ultrasound reveals viable vessels hidden beneath the surface.
Pediatrics and neonatology:
Children often have very small veins that are hard to locate. Additionally, children may experience pain and anxiety while undergoing multiple attempts at cannulation. Real-time imaging makes obtaining IV access in children faster, safer, and less traumatic.
Pre-op and anesthesia:
Reliable IV access is a prerequisite for surgery and anesthesia. Ultrasound ensures timely access without planning or implementing more difficult procedures.
Looking ahead: next steps
Ultrasound-guided IV access is more than a procedural upgrade—itʼs a paradigm shift in patient care. The evidence is clear: this approach increases success, decreases complications, and prevents the cascade of interventions that too often follow multiple failed attempts at venous access.
Multiple professional societies endorse USGIVA. The evidence reveals significant benefits. Moreover, clinicians who adopt the use of ultrasound for PIV never look back. Whether managing a high-acuity emergency department or supporting patients through long-term treatment, USGPIV can elevate the quality and consistency of care.
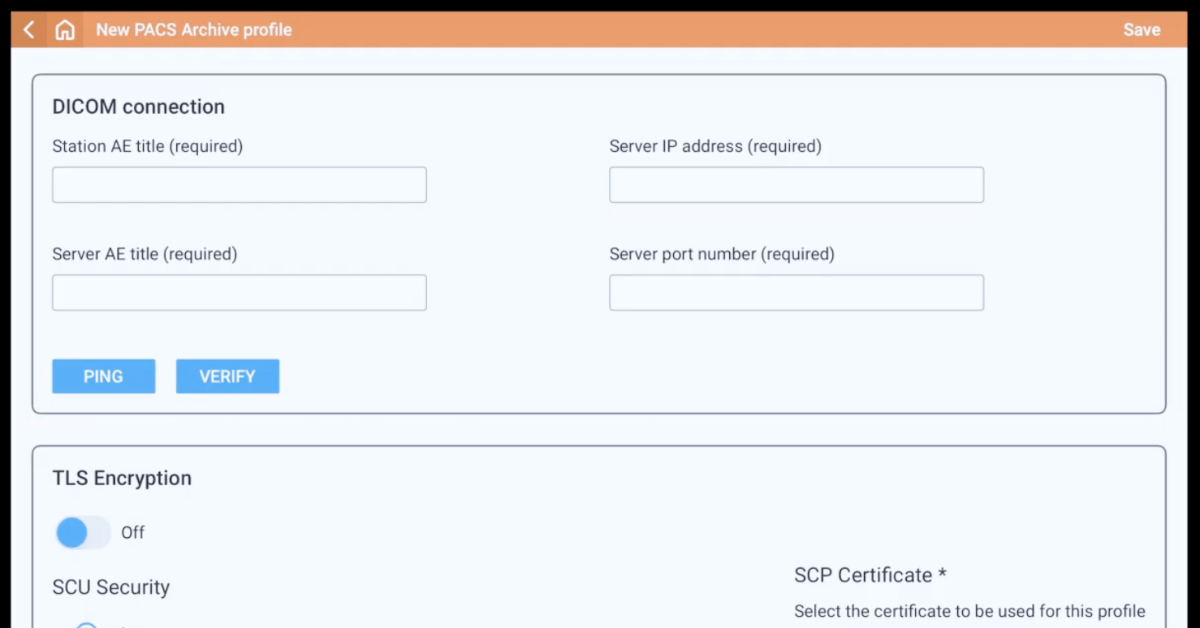
Letʼs talk about implementation
Curious about how to get started—or how to expand an existing ultrasound-guided IV program?
Our team can help with:
• Device selection and comparison
• Training options
• Workflow optimization
• Scaling across multiple departments
FAQs
USGIVA is a technique where a clinician uses real-time ultrasound imaging to see the patient’s veins. This image allows them to guide the IV needle with precision, leading to quicker and more successful cannulation, especially in difficult cases.
Placing a traditional IV can be difficult in many patients. As many as 30% of adults and 50% of children have difficult venous access (DVA), and 35-50% of all traditional IV attempts fail. This can lead to multiple painful needle sticks, delays in care, and potential complications.
Yes. Evidence shows USGIVA significantly boosts first-attempt success rates. One meta-analysis found a nearly four-fold increase in success, while another showed a twice-higher likelihood of first-attempt success. A pediatric study found a 90% first-pass success rate with ultrasound compared to just 18% with the traditional method.
While it can be used for any patient, it is especially valuable for patients with difficult venous access (DVA). This includes:
– Patients with obesity or edema
– Patients who are dehydrated or hypotensive
– Patients with a history of IV drug use, chemotherapy, or hemodialysis
– Pediatric and neonatal patients, who have very small veins
– Patients who have already had multiple failed traditional IV attempts
The primary patient benefits include:
– Fewer needle sticks and less discomfort.
– Faster time to successful IV placement (one pediatric study showed 6.3 minutes vs. 14.4 minutes for traditional).
– Lower risk of complications like hematomas, arterial punctures, and phlebitis.
– Higher overall satisfaction with their care.
Yes. One of the most important benefits of USGIVA is its ability to reduce the unnecessary escalation to a central venous catheter (CVC) or PICC line. By gaining reliable peripheral IV access, clinicians can often avoid the CVC, which carries much higher risks of serious complications (like bloodstream infections) and is significantly more costly.
Yes. Leading organizations, including the Infusion Nurses Society (INS), the American College of Emergency Physicians (ACEP), and the Agency for Healthcare Research and Quality (AHRQ), all endorse or recommend using ultrasound for vascular access, particularly for patients with DVA, to improve safety and outcomes.
Yes. By preventing the need for costly central lines and reducing complications, USGIVA saves money. The text cites one study that found the ultrasound group saved an average of over $83 per patient. Furthermore, avoiding a single central line-associated bloodstream infection (CLABSI) can save tens of thousands of dollars.
It is widely used across many departments. While critical in Emergency Departments and Intensive Care Units (ICUs), it is also standard practice in oncology, pediatrics/neonatology, and pre-op/anesthesia to ensure reliable access for treatment and surgery.
Ask us today for more information on implementing a cost-effective USGIVA program at your facility.
References
- Gorski LA, Hadaway L, Hagle ME, et al. Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs. 2021;44(1S Suppl 1):S1-S224. doi:10.1097/NAN.0000000000000396
- American College of Emergency Physicians. Emergency Ultrasound Guidelines. Annals of Emergency Medicine. 2009;53(4):550-570.
- AIUM. (2019, February 13). AIUM Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures. https://onlinelibrary.wiley.com/doi/10.1002/jum.14954
- Stolz LA, Stolz U, Howe C, Farrell IJ, Adhikari S. Ultrasound-Guided Peripheral Venous Access: A Meta-Analysis and Systematic Review. The Journal of Vascular Access. 2015;16(4):321-326. doi:10.5301/jva.5000346
- Tran QK, Fairchild M, Yardi I, Mirda D, Markin K, Pourmand A. Efficacy of Ultrasound-Guided Peripheral Intravenous Cannulation versus Standard of Care: A Systematic Review and Meta-analysis. Ultrasound Med Biol. 2021;47(11):3068-3078. doi:10.1016/j.ultrasmedbio.2021.07.002
- D’Alessandro M, Ricci M, Bellini T, et al. Difficult Intravascular Access in Pediatric Emergency Department: The Ultrasound-Assisted Strategy (DIAPEDUS Study). J Intensive Care Med. 2024;39(3):217-221. doi:10.1177/08850666231199050
- Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. doi:10.1097/NAN.0000000000000100
- Malik A, Dewald O, Gallien J, et al. Outcomes of Ultrasound Guided Peripheral Intravenous Catheters Placed in the Emergency Department and Factors Associated with Survival. Open Access Emerg Med. 2023;15:177-187. Published 2023 May 19. doi:10.2147/OAEM.S405692
- CipherHealth. (2025, March 13). How to boost patient satisfaction and HCAHPS scores. Retrieved from https://onlinelibrary.wiley.com/doi/10.1002/jum.14954
- Results. Content last reviewed November 2017. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/hai/pfp/haccost2017-results.html
- Haddadin Y, Annamaraju P, Regunath H. Central Line–Associated Blood Stream Infections. [Updated 2022 Nov 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
- Hadaway L. Short peripheral intravenous catheters and infections. J Infus Nurs. 2012;35(4):230-240. doi:10.1097/NAN.0b013e31825af099
- Bahl, A., Xing, Y., Gibson, S. M., & DiLoreto, E. (2024). Cost effectiveness of a vascular access education and training program for hospitalized emergency department patients. PLOS ONE, 19(10), e0310676. https://doi.org/10.1371/journal.pone.0310676
- Stuckey C, Curtis MP. Development of a nurse-led ultrasound-guided peripheral intravenous program. J Vasc Nurs. 2019;37(4):246-249. doi:10.1016/j.jvn.2019.07.003
- Shokoohi H, Boniface K, McCarthy M, et al. Ultrasound-guided peripheral intravenous access program is associated with a marked reduction in central venous catheter use in noncritically ill emergency department patients. Ann Emerg Med. 2013;61(2):198-203. doi:10.1016/j.annemergmed.2012.09.016
- Fields JM, Piela NE, Au AK, Ku BS. Risk factors associated with difficult venous access in adult ED patients. Am J Emerg Med. 2014;32(10):1179-1182. doi:10.1016/j.ajem.2014.07.008