Peripheral Vascular Emergencies: Mastering POCUS for Rapid Diagnosis in the ED
Amid the frenetic bustle of the ED, peripheral vascular emergencies such as deep vein thrombosis (DVT), venous thromboembolism (VTE), and acute hematoma require prompt, accurate diagnosis to avoid life-altering complications.
Consider a patient with swelling and pain in the leg—is it a hematoma, clot, or something else?
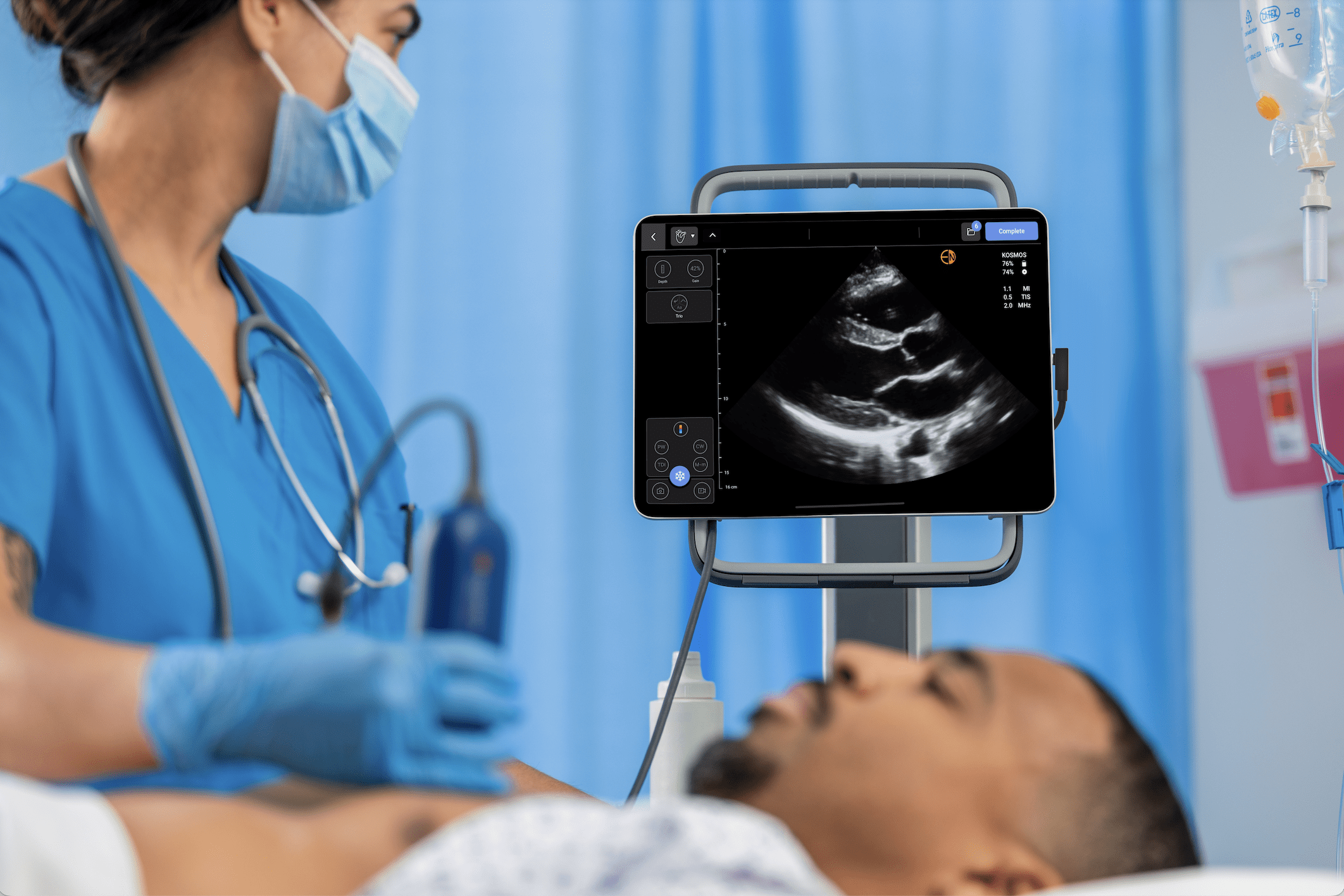
Point-of-care ultrasound (POCUS) is your essential diagnostic tool, delivering instant information without the delay of conventional imaging. With the help of technologies such as compression ultrasound and lower extremity ultrasound, ED physicians can diagnose DVT, evaluate hematomas, and direct life-saving interventions in minutes.
This article serves as an overview on POCUS proficiency in diagnosing peripheral vascular emergencies, from the evidence to the tips.
From recognizing the non-compressible vein to observing the faintly visualized sign of a hematoma, use ultrasound to turn uncertainty into action, whether you are an ED veteran or merely a novice learning POCUS.
Read more about how ultrasound has become essential in emergency medicine, expediting triage and diagnosis to reduce morbidity and mortality in critically ill patients.
Key Takeaways
- Comprehensive Overview of DVT Diagnosis: Deep vein thrombosis compression ultrasound diagnosis is greater than 95% sensitive, guiding early anticoagulation
- Decrease Risk for VTE: POCUS can diagnose DVT, an essential part of venous thromboembolism, thereby averting the evolution into pulmonary embolism
Hematoma Detection: Ultrasound of hematoma discriminates collections of blood from other fluid masses and facilitates management of trauma - Lower Extremity Mastery: During a complete vascular examination, lower extremity ultrasound identifies veins, arteries, and soft tissue
- Bedside Efficiency: POCUS yields immediate, non-invasive diagnoses that reduce delay times and enhance ED treatment
Table of contents
- Peripheral Vascular Emergencies: Mastering POCUS for Rapid Diagnosis in the ED
- Why POCUS is Important in Peripheral Vascular Emergencies
- Deep Vein Thrombosis: Rapid Diagnosis using POCUS
- Venous Thromboembolism: The Bigger Picture
- Ultrasound of Hematomas: How to Identify and Interpret Fluid Collections
- Lower Extremity Ultrasound: A Practical Overview
- Case Studies: POCUS in Action
- Training and Competency for ED Physicians
- Future Directions: Advancing POCUS in Vascular Care
- Frequently Asked Questions about POCUS for Vascular Emergencies
- Conclusion
- References
Why POCUS is Important in Peripheral Vascular Emergencies
Peripheral vascular emergencies, ranging from DVT to acute arterial occlusion, must be diagnosed early before complications like pulmonary embolism, limb ischemia, or compartment syndrome set in.
In the emergency department, every second counts.
POCUS is rapid, bedside, non-invasive, and radiation-free. With POCUS, compared to CT scan or MRI, with transport time and waiting time, ED physicians can assess at the bedside, and scans can be completed in under 10 minutes. There is evidence to show POCUS decreases the time of diagnosis by as much as 50% in vascular emergencies, and there is a better patient outcome. (1)
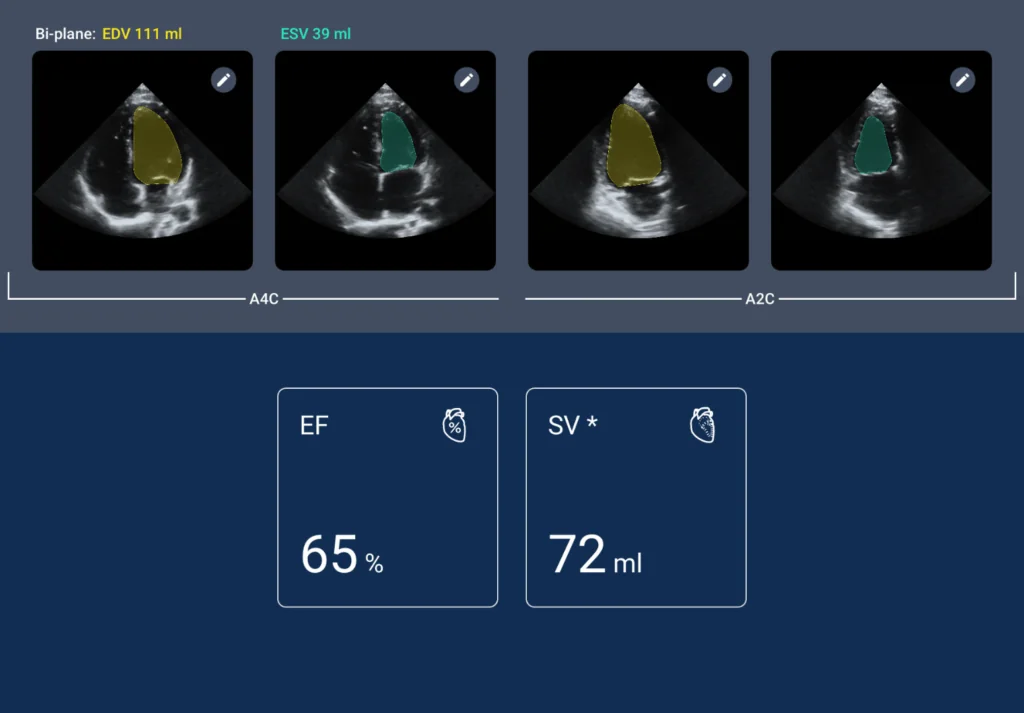
Compression ultrasound for DVT is greater than 95% sensitive and specific, and as good as formal radiologic evaluation. For hematomas, POCUS can detect blood accumulation but not abscess or pseudoaneurysm, and this is what is used to make decisions. Ultrasound of lower extremities looks at veins, arteries, and soft tissue, and can detect the precursors to venous thromboembolism or trauma. With the use of point-of-care technology like Kosmos, ED physicians can now incorporate POCUS in full, and it’s the new standard of practice. (2)
Deep Vein Thrombosis: Rapid Diagnosis using POCUS
Understanding DVT and Its Risk
Deep vein thrombosis (DVT) is the occurrence of blood clots in deep veins, usually in the legs. Untreated DVT leads to venous thromboembolism (VTE), including pulmonary embolism (PE), with 5% mortality at 1 month and 10% at 1 year, twice as high for PE.
Post-thrombotic syndrome develops in up to 50% of DVT patients, with chronic pain and swelling. Early detection of DVT is thus crucial in the ED to permit anticoagulation and prevent complications.
Compression Ultrasound for DVT Diagnosis
Compression ultrasonography is the gold standard for the diagnosis of DVT with high accuracy, safety, and efficiency. POCUS, as performed by an ED doctor, is 96% sensitive and 97% specific and has been proven to be a reasonable trade-off versus radiology studies. It is particularly useful in EDs that lack 24/7 imaging, in which delays in time lead to missed diagnoses, especially since fewer than 30% of high-risk patients will return for outpatient imaging. (3)
Protocols and Techniques
There are several POCUS protocols for DVT detection:
- 2-Point Protocol: Examines the common femoral vein (CFV) and popliteal vein (PV).
- 2-Region Protocol: The same, but can miss isolated femoral vein thromboses.
- 3-Region Protocol (Extended Compression Ultrasound): Examines the CFV, femoral vein, and PV, which is recommended for its complete coverage.
The 3-region protocol is used to find isolated femoral vein clots. Steps are:
- Positioning: Supine for femoral veins; external hip rotation and knee flexion for PV.
- Transducer: Linear probe (7-12 MHz) for superficial veins; phased array or curvilinear (2-5 MHz) for deeper structures.
- Technique: Compress the veins transversely every 1-2 cm from the CFV (below the inguinal ligament) to the PV. A normal vein will completely collapse; non-compressibility is indicative of DVT.
Ultrasound Findings
- Acute DVT: Anechoic or hypoechoic intraluminal defect, typically soft and compressible.
- Chronic DVT: Hyperechoic, calcified thrombus secondary to fibrosis.
- Doppler: Spectral or color Doppler can be used to establish flow obstruction, but compression may suffice in the ED.
Pitfalls and Limitations
- Operator Dependence: Requires training to avoid errors.
- Non-Compressible Mimics: Lymph nodes, Baker’s cysts, or tumors can imitate DVT.
- Calf Veins: May be neglected unless imaged specifically, but their clinical relevance is debated.
With practice, ED physicians can eliminate these obstacles, offering accurate DVT diagnosis.
Venous Thromboembolism: The Bigger Picture
Linking DVT to VTE
Venous thromboembolism (VTE) encompasses DVT and PE, with DVT commonly resulting in PE. The significant morbidity of VTE—a 5% 1-month mortality rate for DVT, which doubles for PE—renders swift diagnosis imperative. Post-thrombotic syndrome develops in as many as 50% of patients with DVT and causes chronic venous insufficiency. In the ED, the prompt recognition of DVT prevents VTE progression. (4)
POCUS in VTE Management
POCUS is better in detecting DVT, which is a core VTE component. While it does not directly diagnose PE, ruling out DVT renders PE less probable as the etiology of symptoms. In PE suspicion, other ultrasound views (e.g., right ventricular strain) can provide indirect information but remain secondary to vascular examination in the periphery. POCUS’s ability to diagnose DVT makes immediate anticoagulation possible and reduces VTE-related complications.
Ultrasound of Hematomas: How to Identify and Interpret Fluid Collections
What Are Hematomas and How Are They Formed?
A hematoma is a pocket of blood that forms outside of blood vessels. This can happen following trauma, during or after a medical procedure, or in patients taking blood thinner medications.
For acute care—trauma or vascular access cases, in particular, hematomas will form following an arterial puncture or from blunt trauma. Sometimes the pressure of the blood can affect surrounding veins or even nerves, resulting in additional problems if not addressed early. (5)
What Hematomas Look Like on Ultrasound
Acute or newer hematomas are disorganized in appearance on the scan. The collection on the screen is seen as a mix of dark (anechoic) and light grayish (hypoechoic) zones, occasionally with strands or clumps within it—those represent fibrin or clot elements. The edges of the collection aren’t usually well defined.
Chronic hematomas, the longstanding ones, start to become more differentiated. They’re brighter (hyperechoic) and better for outlining.
In addition, one of the useful aspects of ultrasound is doppler imaging, which detects blood flow. Hematomas don’t have internal flow, so they can be identified as distinct from such things as pseudoaneurysms. Pseudoaneurysms will usually show swirling blood flow, which some refer to as the “yin-yang” pattern.
Ultrasound also helps to differentiate hematomas from other fluid collections:
- Abscesses usually have thick edges and appear darker (hypoechoic), with air inside them sometimes.
- Seromas appear much neater. They’re usually well-defined and all black (anechoic) on the screen.
- If the problem is active bleeding, contrast-enhanced ultrasound with microbubbles can show that. This helps with treatment, for example, by showing where to inject thrombin to stop the bleed.
Why Hematomas Matter Clinically
Hematomas are more than just cosmetic problems. They become dangerous when they continue to grow, particularly in small spaces where they press against the tissues surrounding them. This causes compartment syndrome, which must be treated immediately. When trauma or vessel injury occurs, the presence of a hematoma also indicates internal bleeding or vessel trauma.
That’s where point-of-care ultrasound (POCUS) comes in. It’s quick, portable, and helpful both for checking if a hematoma is getting bigger and for guiding procedures like draining the collection.
Lower Extremity Ultrasound: A Practical Overview
Where to Look: Key Anatomical Points
When performing an ultrasound on the lower limbs, you’re mostly scanning veins, arteries, and soft tissue. Some key landmarks to be aware of:
- Common Femoral Vein (CFV): Runs just medial to the common femoral artery, just above the groin (inguinal ligament).
- Femoral Vein: Runs parallel with the femoral artery down the thigh.
Popliteal Vein (PV): Behind the knee, just medial to the popliteal artery.
How to Scan and What to Observe
Below is a rough outline for a systematic scan:
- Venous Exam: Observe CFV, femoral vein, and PV. With compression US, observe DVT. In case a vein does not compress, there would be a clot.
- Arterial Exam: Less accessible in an emergency scenario, but useful to detect a block or an aneurysm.
- Soft Tissue Survey: Detect fluid collections like hematomas, abscesses, or Baker’s cyst.
Key Pathologies
Some of the results you might have are:
- Deep Vein Thrombosis (DVT): The vein will not be compressible, and there may be a darker (hypoechoic) clot present.
- Hematoma: A mixed (heterogeneous) collection of fluid.
- Abscess: A darker fluid with thick walls, sometimes with small gas bubbles.
- Baker’s Cyst: A nice-appearing fluid collection behind the knee. It’s anechoic and usually well-defined, which can be used to distinguish it from a DVT based on location alone.
Despite what the 2024 ESC Guidelines claim—restricting POCUS’s role in quick vascular evaluation—clinicians nonetheless find it a valuable and handy tool to properly and quickly evaluate lower limb complications. (6)
Case Studies: POCUS in Action
Case 1: A Suspected Yet Significant DVT
A 50-year-old woman presented with severe swelling and striking pain in her right leg subsequent to an overseas flight of considerable length. Through the utilization of a thorough three-region ultrasound protocol, point-of-care ultrasound demonstrated an incompressible popliteal vein, effectively validating the diagnosis of deep vein thrombosis. Initiation of appropriate anticoagulation medication and admission for ongoing observation were undertaken to forestall the possibility of a potentially catastrophic pulmonary embolism.
Case 2: Deciphering the Etiology of Post-Traumatic Thigh Pain
A physically fit yet concerned 35-year-old male reported considerable pain in his thigh in the aftermath of an alarming motorbike collision. Application of point-of-care ultrasound revealed an irregular anechoic structure within the soft tissues of the anterior thigh, devoid of doppler flow signals, consistent with the formation of a hematoma.
Exploration using ultrasound excluded the presence of concurrent deep vein thrombosis. Admission for conservative management and follow-up evaluation was deemed most suitable in this case.
Training and Competency for ED Physicians
Building POCUS Skills
Vascular POCUS expertise requires:
- Formal Training: Consider ACEP or SCCM courses, with vascular modules
- Guided Practice: 25-50 scans to achieve proficiency
- Ongoing Use: Periodic scanning is used to update skills
The American College of Emergency Physicians places a priority on credentialing and quality assurance for POCUS competency.
Guidelines and Resources
- ACEP Ultrasound Guidelines: Outline POCUS applications, including vascular emergencies
- Society for Vascular Surgery: Provides protocols for DVT assessment
Future Directions: Advancing POCUS in Vascular Care
Emerging Technologies
- AI-Assisted POCUS: Algorithms enhance image interpretation, reducing errors.
- Automated Compression Devices: Normalize DVT detection.
- Portable Probes: Kosmos and other devices increase accessibility.
Check out Kosmos AI and Kosmos Ultraportable Ultrasound to find out more about how EchoNous is changing the world of emergency medicine!
Integration with Other Modalities
Combining POCUS with D-dimer testing or CT angiography can make complex diagnoses. 2024 ACC/AHA Guidelines suggest combining POCUS with lab tests for comprehensive vascular assessment.
Frequently Asked Questions about POCUS for Vascular Emergencies
- How useful is POCUS for diagnosing DVT?
POCUS is extremely accurate, both in sensitivity and with a specificity of more than 95%. That is, it is as close to matching the results you would get from traditional radiology imaging, but it can be done so much faster at the bedside.
- Can POCUS directly diagnose a pulmonary embolism (PE)?
Not exactly. It can’t pick up a PE itself, but it’s great at picking up DVT, which often leads to PE. Also, it can pick up markers that suggest strain on the right side of the heart — a sure sign that a PE may be happening.
- How is a hematoma ultrasound different from one for DVT?
A hematoma does not compress and may look irregular or mottled on the image. A DVT will show a vein that does not compress and has a clot.
- What training is needed to do a lower extremity ultrasound?
You’ll need to take a structured course, get supervised hands-on practice, and use the technique regularly to stay sharp. That combination helps ensure you’re doing it right and getting accurate results.
- Is POCUS a cost-effective option in the emergency department?
Definitely. It saves money by cutting down on more expensive tests and shortens the time patients wait for answers. That means quicker treatment and better flow in a busy ER.
Conclusion
Point-of-care ultrasound, or POCUS, is changing the way vascular crises are treated by emergency rooms. Deep vein thrombosis (DVT), venous thromboembolism (VTE), and internal bleeding or hematomas are among the conditions to which it lends itself particularly well.
POCUS is unnecessary for doctors who can act on their feet quickly with tools like compression ultrasound and lower limb scans. Thus, Ellipsis CT helps in the early detection of hematoma due to trauma, helping in management before the patient deteriorates.
The regular use of POCUS helps emergency teams identify important problems promptly, minimizes complications, and enhances outcomes for patients who otherwise might be at heightened risk. Tap the potential of POCUS with Kosmos by EchoNous and request a demo today.
References
- Drake, A., Dreyer, N., Hoffer, M., & Boniface, K. (2022). Point-of-care Ultrasound for the Evaluation of Acute Arterial Pathology in the Emergency Department: A Case Series. Clinical practice and cases in emergency medicine, 6(1), 1–7. https://doi.org/10.5811/cpcem.2021.11.54904
- Frederick, M. K., Stolz, L. A., & Duran-Gehring, P. E. (2024). Vascular Ultrasound. Emergency medicine clinics of North America, 42(4), 805–818. https://doi.org/10.1016/j.emc.2024.05.011
- Zuker-Herman, R., Ayalon Dangur, I., Berant, R., Sitt, E. C., Baskin, L., Shaya, Y., & Shiber, S. (2018). Comparison between two-point and three-point compression ultrasound for the diagnosis of deep vein thrombosis. Journal of thrombosis and thrombolysis, 45(1), 99–105. https://doi.org/10.1007/s11239-017-1595-9
- Roberts, L. N., & Arya, R. (2011). Deep vein thrombosis and pulmonary embolism: diagnosis, treatment and prevention. Clinical medicine (London, England), 11(5), 465–466. https://doi.org/10.7861/clinmedicine.11-5-465
- Liu, J. L., Li, J. Y., Jiang, P., Jia, W., Tian, X., Cheng, Z. Y., & Zhang, Y. X. (2020). Literature review of peripheral vascular trauma: Is the era of intervention coming?. Chinese journal of traumatology = Zhonghua chuang shang za zhi, 23(1), 5–9. https://doi.org/10.1016/j.cjtee.2019.11.003
- Barros, F. S., Storino, J., Cardoso da Silva, N. A., Fernandes, F. F., Silva, M. B., & Bassetti Soares, A. (2024). A comprehensive ultrasound approach to lower limb varicose veins and abdominal-pelvic connections. Journal of Vascular Surgery. Venous and lymphatic disorders, 12(3), 101851. https://doi.org/10.1016/j.jvsv.2024.101851