A Guide to Bladder Scanners: Technology, Use Cases, and AI
Table of Contents
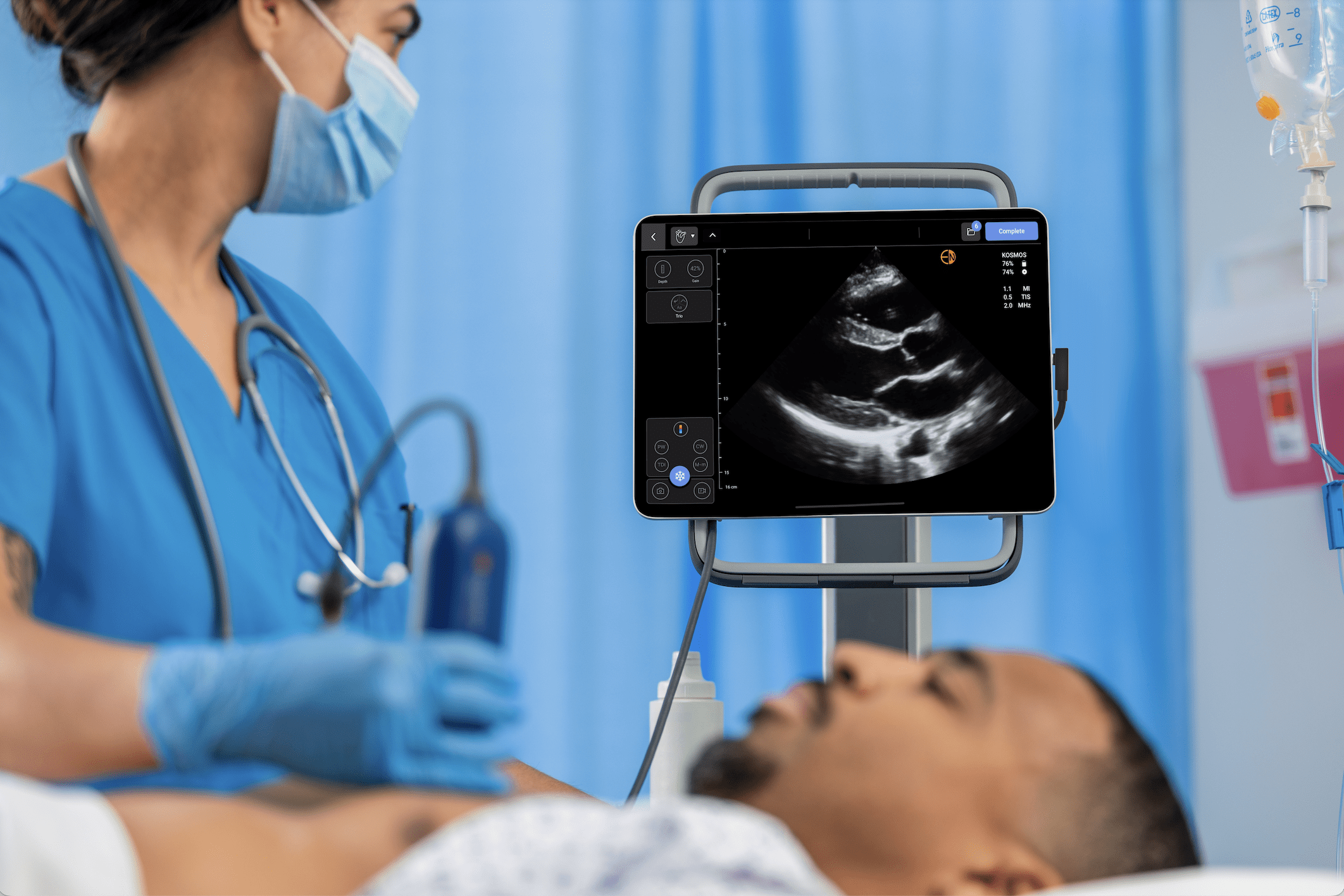
Point-of-care ultrasound (POCUS) has changed how medicine is practiced by allowing clinicians to see inside the human body at the bedside. For nurses, one of the most practical applications of this technology is the modern bladder scanner. The assessment method has evolved from a subjective guess based on palpation to a rapid, data-driven process that enhances patient safety, prevents unnecessary procedures, and improves nursing workflows.
This guide covers the essentials of bladder scanning technology, its role in patient care, and how advancements like artificial intelligence contribute to the current standard of care in nursing.
What Is a Bladder Scanner?
A bladder scanner is a specialized, non-invasive portable ultrasound device designed to measure the volume of urine in a patient’s bladder. Previously, nurses relied on inexact methods like palpation or percussion to detect a full bladder. The bladder scanner replaces this guesswork with objective data, providing a quick and reliable way to determine bladder volume, particularly Postvoid Residual (PVR)—the amount of urine left after urination.
This objective measurement is a key component of evidence-based nursing practice. It provides quantitative feedback that helps clinicians assess bladder emptying and determine if intervention is needed. While no single definition is standardized, a PVR volume greater than 200 mL is considered a sign of inadequate emptying, with some sources defining urinary retention at volumes over 300 mL or 400 mL.1 This information makes the bladder scanner a crucial tool for reducing Catheter-Associated Urinary Tract Infections (CAUTIs) by helping avoid unnecessary catheterizations.
Bladder Scanners: A Specialized Ultrasound Device
The technology inside an ultrasound probe is a key differentiator that impacts performance. At the core of any ultrasound probe are piezoelectric crystals. These materials have a unique property: they vibrate to create sound waves when an electric voltage is applied, and conversely, they generate an electric voltage when returning sound waves (echoes) strike them. The ultrasound system’s computer then translates these electrical signals into an image. Key differences among probe types lie in how these crystals are arranged and used to build the final image.
Mechanical Probes
Older bladder scanners often use a mechanical probe. This design typically contains a single piezoelectric crystal that is physically moved by a motor inside the probe housing to sweep across the bladder. This reliance on physical movement can be relatively slow, and the mechanical parts can be noisy and may wear out over time. Any motion of the probe by the person conducting the scan can interfere with the motor’s sweep, potentially leading to inaccurate measurements.
Phased Array Probes
Modern devices, including Kosmos Bladder, use a more advanced electronic phased array probe. Instead of one moving crystal, this type of probe contains an array of many tiny piezoelectric crystals. The scanner electronically “steers” the ultrasound beam across the bladder by sending electrical pulses to the crystals in precisely timed sequences, known as phases. Because there are no moving parts, image acquisition is nearly instantaneous, allowing for real-time visualization. This design is also more durable, operates silently, and is more resistant to motion artifacts, which results in a more accurate and reliable measurement.
Clinical Applications and Use Cases in Nursing
Bladder scanning has applications across numerous departments and patient populations, directly impacting daily nursing care. A primary use is preventing unnecessary catheterization. This single intervention has been shown in studies to reduce unnecessary catheterizations by 16% to 47% and lower associated UTI rates by 38% to 72%.2 In settings like Med-Surg and post-operative units, a quick scan can confirm if a patient’s bladder is truly full, helping nurses avoid an invasive procedure and its risks.
The scanner is also a key diagnostic tool for managing urinary retention and measuring PVR volume. By scanning a patient after they urinate, nurses can determine if the bladder is emptying completely. A high PVR can indicate the need for further intervention and helps in managing ongoing bladder issues. This objective data is also essential for developing evidence-based nursing protocols for bladder management, voiding trials, and post-catheter removal care.
Furthermore, the non-invasive nature of bladder scanning significantly improves the patient experience. Studies and clinical reports indicate that patients prefer it over catheterization because it preserves dignity and reduces discomfort, avoiding the trauma related to urinary tract catheterization.2 This is especially valuable in pediatric populations, where a scan avoids the trauma associated with catheterizing a child who may have difficulty communicating symptoms.1
Why Accuracy and Ease of Use Matter in Nursing
In a clinical setting, a tool’s effectiveness depends on its reliability and adoption by staff.
Accuracy is critical. While intermittent catheterization is considered the gold standard for a precise PVR measurement, multiple studies have concluded that portable bladder ultrasound provides an acceptable level of accuracy for clinical decision-making.2 An overestimated volume might lead to an unnecessary catheterization, while an underestimated volume could result in a missed diagnosis of urinary retention. It’s also important for nurses to be aware of factors that can interfere with accuracy, such as severe abdominal scarring, morbid obesity, or pregnancy.
Ease of use affects adoption, which is critical for nursing leaders. A device with a steep learning curve or cumbersome workflow may be underutilized, leading to inconsistent practice. A scanner that is intuitive and simple to operate ensures consistent adoption across all shifts and among staff with varying levels of technical comfort. This is essential for successfully implementing new institutional protocols.
What Is the Role of AI in Modern Bladder Scanning?
A significant development in bladder scanning technology is the integration of artificial intelligence (AI). AI algorithms are trained on thousands of images to automate and improve the measurement process. This technology is used in the Kosmos platform by EchoNous.
AI contributes to bladder scanning in several ways:
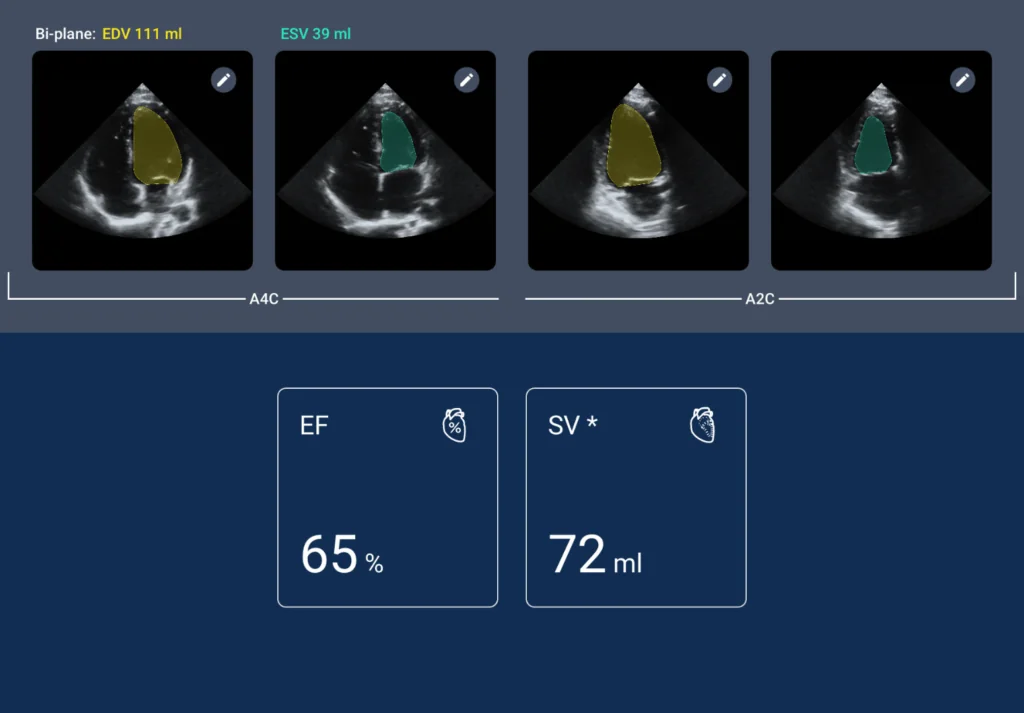
- Automated Bladder Detection: AI can help identify the bladder on the screen, assisting the user in positioning the probe correctly for an optimal measurement.
- Precise Boundary Delineation: An accurate volume calculation depends on correctly defining the bladder walls. AI can automatically trace the bladder’s outline for a more accurate and repeatable calculation.
- Bladder Volume Assessment: The Kosmos system’s AI provides accurate bladder volume measurements, without the user needing to do manual calculations.
For nursing leaders, another benefit of AI is the reduction in user variability, which helps ensure a consistent standard of care and measurement accuracy across the entire nursing staff. By combining an ultrasound probe with AI, the Kosmos Bladder provides not just a number, but a high-fidelity image, giving nurses more confidence in their assessment.
A Tool for Better Nursing Care
The evolution of bladder scanners from mechanical probes to AI-powered electronic arrays shows how technology can support safer, more efficient nursing care. By providing immediate, objective data, these devices empower nurses to make confident, informed decisions at the bedside. For nursing leaders focused on quality improvement and patient safety, the modern AI-powered bladder scanner is an essential tool for implementing best practices. Furthermore, studies indicate that portable bladder ultrasound is a cost-effective technology because it avoids costs associated with catheterization equipment, saves nursing time, and reduces expenses related to treating catheter-related complications and UTIs.
To learn more about how Kosmos Bladder integrates into your nursing workflow, providing best-in-class accuracy to assist with bladder assessment, connect with a clinical product expert or request a personalized demo today.
References
- Ballstaedt L, Leslie SW, Woodbury B. Bladder Post Void Residual Volume. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Updated February 28, 2024. Accessed August 19, 2025 https://www.ncbi.nlm.nih.gov/books/NBK539839/
- Medical Advisory Secretariat. Portable Bladder Ultrasound: An Evidence-Based Analysis. Ontario Health Technology Assessment Series. 2006;6(11). Toronto, ON: Ministry of Health and Long-Term Care; 2006. Accessed August 19, 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC3379524/