Essential Ultrasound Protocols for Critically Ill Patients: EFAST, RUSH, and SHoC-ED
In critical care, time isn’t just valuable—it’s everything. When a patient experiences cardiac arrest or shock, there’s no time to lose. Clinicians need instant answers, and that’s exactly where point-of-care ultrasound (POCUS) shines. At the bedside, it delivers rapid, reliable information that guides the most critical, life-saving decisions.
Protocols like EFAST, the RUSH exam, SHoC-ED, and Cardiac Arrest Ultrasound provide clinicians frameworks to identify life-threatening issues—pneumothorax, IVC collapse, cardiac tamponade—in minutes, without the delay of traditional imaging. At the bedside, ultrasound allows physicians to identify a barcode sign or assess a patient’s volume status with speed and precision.
This article distills these must-know POCUS protocols, offering step-by-step outlines, clinical pearls, and evidence-based guidance to give you confidence when it counts. Whether you work in the ED, or ICU, familiarity with these tools can make chaos clear—and be the difference maker when every moment counts.
Key Takeaways:
- EFAST Accuracy: EFAST ultrasound rapidly detects trauma-related pathologies like pneumothorax, hemoperitoneum, and tamponade with great specificity to direct emergent intervention.
- RUSH Clarity: RUSH protocol categorizes shock by assessment of the heart, volume status, and vessels to allow for rapid discrimination for hypovolemic, cardiogenic, obstructive, or distributive etiologies.
- SHoC-ED Efficiency: SHoC-ED’s tiered approach places utmost priority on central opinions for arrest and hypotension, effective diagnosis in chaotic emergency settings.
- Cardiac Arrest Insight: Arrest ultrasound for reversible conditions like tamponade or pulmonary embolism maximizes outcome without CPR disruption.
- IVC and Barcode Sign Mastery: IVC collapse identifies signs of hypovolemia, and the barcode sign establishes pneumothorax, the essence of real-time decision-making.
Table of contents
- Essential Ultrasound Protocols for Critically Ill Patients: EFAST, RUSH, and SHoC-ED
- Why Ultrasound Matters in Critical Care
- EFAST Ultrasound: Your Trauma Toolkit
- RUSH Protocol: Decoding Shock
- SHoC-ED Protocol: Rapid, Focused Approach in Emergencies
- Ultrasound in Cardiac Arrest: Real-Time Help When Seconds Count
- Choosing the Right Protocol for the Situation
- Frequently Asked Questions on Ultrasound Protocols
- Conclusion
- References
Why Ultrasound Matters in Critical Care
Ultrasound’s growing role in critical care isn’t just a trend—it’s a response to the need for faster, safer, and more adaptable tools. Unlike CT scans, which involve radiation exposure and the risks of transporting unstable patients, point-of-care ultrasound (POCUS) offers immediate answers right at the bedside. Studies have shown that in trauma scenarios, ultrasound can reduce diagnostic delays by nearly half—a game-changer when minutes matter.
Its non-invasive nature also allows for repeated checks, which is vital when managing fluctuating conditions like shock or cardiac arrest. Protocols such as EFAST and the RUSH exam help streamline evaluations, enabling clinicians to quickly uncover the root of hypotension or internal injuries.
Spotting a pneumothorax via the barcode sign or identifying IVC collapse can lead directly to life-saving interventions like fluid resuscitation or chest tube placement. Evidence suggests POCUS can boost diagnostic accuracy in shock cases by up to 40% compared to standard assessments.
Beyond diagnostics, it’s an invaluable procedural aid—helping guide everything from pericardiocentesis to vascular access, all while helping minimize complications. And in settings where CT or MRI just aren’t options, ultrasound proves its worth as a cost-effective, portable solution. It’s no surprise that this technology has become an essential tool in emergency rooms and intensive care units around the world—empowering clinicians to move faster, act decisively, and ultimately, save more lives. (1)
EFAST Ultrasound: Your Trauma Toolkit
The Extended Focused Assessment with Sonography for Trauma (EFAST) is an essential tool for evaluating trauma patients at the bedside. It’s built to identify life-threatening conditions like internal bleeding and lung collapse within minutes—making it indispensable in critical care and emergency medicine.
What Is EFAST?
EFAST is an extension of the traditional FAST exam with thoracic views, which enables the detection of pericardial effusion, hemoperitoneum, hemothorax, and pneumothorax. It’s highly specific—especially for pneumothorax, where the lung point sign is nearly 100% specific.
It’s less sensitive in small bleeds, so it always has to be used with clinical judgment. One of the best things about EFAST is its rapidity: it can be possible to perform the entire scan in under five minutes, which helps with urgent interventions like surgery or chest tube placement. (2)
Performing EFAST Step-by-Step
EFAST has five fundamental views, each for a specific location:
- Pericardial (Subxiphoid): The probe is placed below the xiphoid process and pointed towards the left shoulder. Anechoic fluid near the heart is sought as an early indicator for tamponade or effusion.
- Right Upper Quadrant (RUQ): The probe is placed over the 8th–11th ribs on the midaxillary line, with the notch pointed to the liver-kidney interface (Morrison’s pouch). Free fluid appears as black, anechoic stripes.
- Left Upper Quadrant (LUQ): This view mirrors the RUQ, targeting the area between the spleen and diaphragm. Fluid in this area may suggest splenic injury.
- Pelvic: The probe is placed just above the pubic symphysis, angled downward. This scans for fluid in the rectovesical (in males) or rectouterine (in females) spaces.
- Pleural (Lung): A high-frequency linear probe is used at the 2nd–4th intercostal spaces in the midclavicular line. Both sides are scanned for lung sliding and pleural effusion.
Apply a curvilinear probe (2–5 MHz) to obtain cardiac and abdominal images, and revert to a linear probe (7–12 MHz) for obtaining lung images. Begin with the pericardial window to rule out tamponade, and then follow in a sequential manner. Maintain your patient in a supine position and adjust depth and gain for an optimal image.
Detecting Pneumothorax: The Barcode Sign
One of EFAST’s key capabilities is pneumothorax detection. Under normal conditions, the visceral and parietal pleura slide against each other—a shimmering motion at the pleural line. In pneumothorax, this sliding disappears.
On M-mode, the result is the barcode sign: evenly spaced horizontal lines, in contrast to the granular seashore pattern of normal lungs. Spotting a lung point, where sliding resumes, confirms pneumothorax with high specificity. Operator experience improves sensitivity, which ranges from 50–90%. (3)
Key Findings and Interpretations
- Free Fluid: Black (anechoic) fluid in the RUQ, LUQ, or pelvic view suggests bleeding—potentially requiring urgent surgical intervention.
- Cardiac Tamponade: Look for pericardial effusion and right ventricular collapse during diastole—classic signs of compromised cardiac output.
- Hemothorax: Fluid visible above the diaphragm, often with the “spine sign,” indicates blood in the pleural space.
- Pneumothorax: Absence of lung sliding, a barcode sign on M-mode, and presence of a lung point are strong indicators.
Pitfalls and Limitations
EFAST is not infallible. Minor fluid accumulations, retroperitoneal trauma, or perforation of the bowel may escape detection. Its sensitivity for intra-abdominal hemorrhage in stable patients can fall to as low as 40%.
The imaging is also limited in the obese or the patient with subcutaneous emphysema. Misinterpretations can happen too—fat can simulate effusion, and pleural fluid can be confused with ascites. Always relate your findings to the clinical scenario, and repeat the scan without hesitation if in doubt.
Clinical Applications
EFAST is a first-line instrument for penetrating and blunt trauma, directing life-saving intervention like laparotomy or thoracostomy. It can also be used to diagnose more than trauma—it can be utilized in the diagnosis of ectopic pregnancy, ruptured aneurysm, or even mass casualty triage. In all high-risk contexts, EFAST brings speed, clarity, and confidence to bedside practice.
RUSH Protocol: Decoding Shock
The Rapid Ultrasound for Shock and Hypotension (RUSH) exam is a critical tool in managing patients with undifferentiated shock. In just a few minutes, it can help determine whether the cause is hypovolemic, cardiogenic, obstructive, or distributive—streamlining treatment when time is of the essence.
What Is RUSH?
RUSH splits the evaluation into three parts: the pump (cardiac), the tank (abdominal and volume status), and the pipes (large vessels). This logical progression enhances diagnostic yield well above clinical expertise. (4)
Step-by-Step RUSH Assessment
The Pump
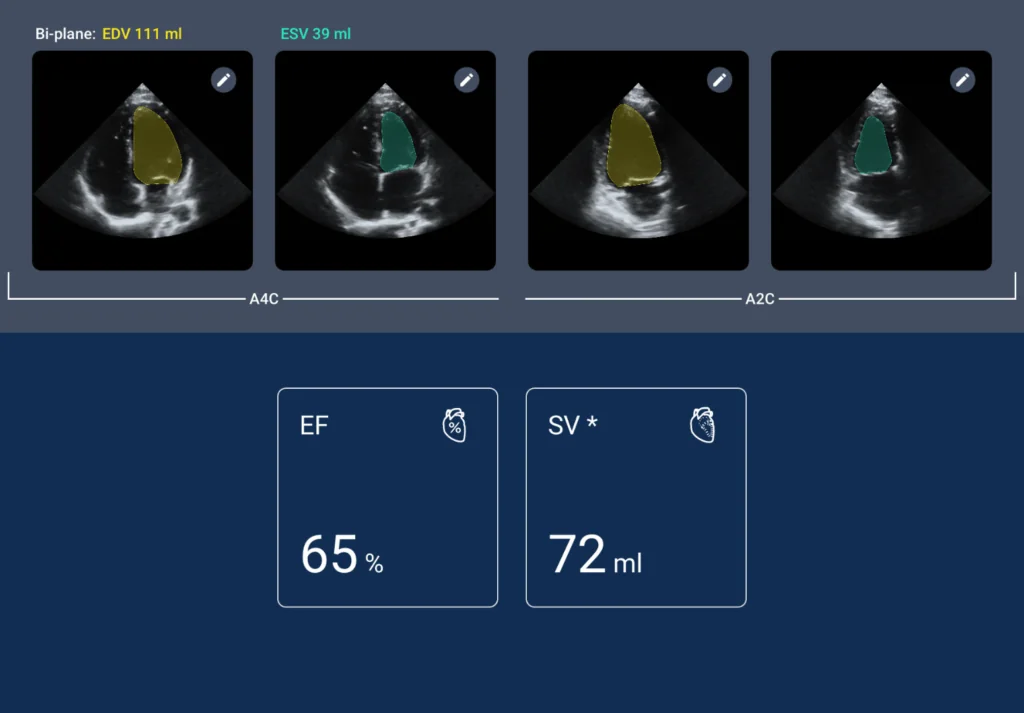
Begin by using a phased-array probe (2–5 MHz) to capture core cardiac views: parasternal long and short axes, subxiphoid, and apical four-chamber. The assessment focuses on:
- Contractility: A heart that’s hyperdynamic may point to sepsis or hypovolemia, while reduced movement suggests a cardiogenic cause.
- Effusion/Tamponade: Look for anechoic fluid and signs of right heart chamber compression.
Right Ventricular Strain: If the right ventricle is seen to be dilated or the left ventricle is D-shaped, suspect pulmonary embolism.
The Tank
Proceed to assess the IVC, abdomen, and lungs:
- IVC: Use a curvilinear probe, 1–2 cm from the junction with the right atrium.
- Abdomen: Scan through the RUQ, LUQ, and pelvis for free fluid—whether blood or ascites.
Lungs: Scan for B-lines, which suggest pulmonary edema, or absent sliding, which could mean a pneumothorax
The Pipes
With the curvilinear probe, assess:
- Aorta: Start from the epigastrium and follow it to the iliac bifurcation. This is done to rule out aneurysm or dissection.
- Leg Veins: Check compressibility of femoral and popliteal veins to spot potential DVTs.
IVC Collapse: A Window Into Fluid Status
Regarding determining a patient’s volume status, the integrity of the inferior vena cava (IVC) is helpful information. Under normal circumstances, the IVC measures 1.5-2.5 cm in diameter and should become half collapsed with spontaneous inspiration. When the collapsibility index is more than 50%, it generally signifies that the patient is hypovolemic and will correct with fluid resuscitation.
A dilated IVC of more than 2.5 cm with less than 20% collapse, however, can imply fluid overload or even obstructive etiologies like tamponade or pulmonary embolism. In adults on mechanical ventilation, a distensibility index of more than 18% is a valid predictor that they will respond to fluids. These findings are even more robust when used in combination with cardiac and lung ultrasound findings. (5)Behind the knee, just medial to the popliteal artery.
Practical Use: Clinical Integration
The RUSH exam shines in the scenario of undifferentiated hypotension. Start with a look at the heart to determine if there are cardiogenic shock findings. Move on to the IVC and abdominal windows. For example, if you notice a small, collapsible IVC with pelvic free fluid—that may be hemorrhagic shock.
If the IVC is distended and there are B-lines in the lungs, think fluid overload or heart failure. Keep in mind, though, chronic diagnoses like pulmonary hypertension can muddy the waters by elevating baseline central pressures.
This is why it is so critical to always merge multiple ultrasound findings and correlate with the patient’s clinical picture. At the end of the day, RUSH is a matter of direction—it dictates whether to push fluids, initiate vasopressors, or try thrombolytics at the bedside.
Case in Point
Suppose a 60-year-old female comes in with tachycardia and hypotension. Her RUSH exam reveals her to have a hyperdynamic heart, flat IVC, and no intra-abdominal fluid—classic for septic shock. She is started immediately on fluids and antibiotics. There is a later lung scan that reveals B-lines, and there is a shift to diuresis because of fluid overload. This example reveals how responsive and adaptable the RUSH protocol may be. It changes depending upon the patient’s condition and is helpful in preparing timely, intelligent decisions regarding treatment.
SHoC-ED Protocol: Rapid, Focused Approach in Emergencies
The SHoC-ED protocol—Sonography in Hypotension and Cardiac Arrest in the Emergency Department—is an organized but flexible system for assessing seriously unstable patients. It’s designed to allow physicians to address the need for rapid decisions without compromising thorough exams.
What is SHoC-ED all about?
SHoC-ED aims to quickly diagnose reversible hypotension and cardiac arrest causes and does so by guiding clinicians through an ordered list of ultrasound views, divided into three groups: core, supplemental, and additional. This structuring keeps things simple, especially in the chaotic pace of emergency settings. (6)
Core and Supplemental Ultrasound Views
Core Views
These are the basic views and can usually be completed in under 3 minutes:
- Subxiphoid Window – Look for signs of cardiac motion, pericardial effusion, or tamponade.
- Parasternal Long-Axis View – Assess the left ventricle’s pumping capability.
- Lung Bases – Look for B-lines suggesting pulmonary edema or pleural effusions.
- IVC – Look at size and respiratory variation to estimate volume status.
Supplemental Views
Use if the core views leave unanswered questions:
- Apical Four-Chamber – Useful in confirming or clarifying cardiac findings.
- Pleural Scans – Help establish pneumothorax if lung sliding is absent.
Other Views (If Needed)
- Femoral/Popliteal Veins – Rule out DVT.
- Abdominal Aorta – Exclude aneurysm or dissection if indicated.
Placing It into Practice
The key is to be as fast as possible without taking shortcuts. Start with the basics in early resuscitation. If in doubt, move on to the next step. No lung sliding? A pleural view can confirm a pneumothorax. A distended IVC? Check the heart again for tamponade. Scan the heart and IVC with a phased-array probe and use a linear probe for high-resolution lung views.
Why It Matters
SHoC-ED is especially valuable in the case of hypotension with no apparent etiology. It assists practitioners in deciding whether to give fluids, start vasopressors, or seek obstructive etiologies for shock like tamponade or pulmonary embolism.
In cardiac arrest, it’s a convenient way to rule out or rule in treatable causes. And in sepsis or trauma, its flexibility makes it a must-have. Just keep in mind: this protocol is most effective when core beliefs are second nature—so practice is essential to using it without hindering care.
Ultrasound in Cardiac Arrest: Real-Time Help When Seconds Count
Point-of-care ultrasound (POCUS) during cardiac arrest can offer real-time insight without delaying compressions, helping clinicians make smarter, faster decisions right when it matters most.
Why It Matters in Cardiac Arrest
Ultrasound isn’t just a diagnostic tool—it plays several important roles during resuscitation:
- Prognosis: Seeing cardiac motion is often tied to better chances of recovery.
- Pulse Checks: It can be more reliable than feeling for a pulse by hand.
- Reversible Causes: Quickly spots treatable issues like tamponade, hypovolemia, PE, or tension pneumothorax.
- Procedural Support: Helps guide interventions like pericardiocentesis or needle decompression.
Timing and Technique Tips
Use a phased-array probe during rhythm check pauses—ideally under 10 seconds. Focus on subxiphoid or parasternal windows. Keep an eye out for:
- No Cardiac Motion: Often a poor sign, though not always a reason to stop efforts.
- Effusion with Chamber Collapse: A strong clue for tamponade.
- Enlarged Right Ventricle: Think pulmonary embolism.
- Collapsed IVC: Suggests volume loss.
Some teams are now skilled enough to scan during compressions using subxiphoid views, reducing any breaks in CPR. With enough practice, scanning becomes second nature and doesn’t interfere with ACLS timing.
Spotting the Reversible Hs & Ts
Ultrasound helps quickly zero in on several “Hs and Ts” of cardiac arrest:
- Hypovolemia: Look for a small, fast-contracting heart and a flat IVC.
- Tamponade: Fluid around the heart with signs of compression.
- Tension Pneumothorax: Lack of lung sliding or “barcode sign.”
- Thrombosis (PE): Right heart strain or even a visible DVT.
Take this example: A large pericardial effusion is discovered mid-arrest. Immediate drainage leads to a return of circulation—proving how game-changing ultrasound can be. That said, not every image tells the whole story. Small effusions or tough imaging windows can lead to missed findings. Always consider the full clinical picture. (7)
Case Snapshot
A 45-year-old man collapses with pulseless electrical activity (PEA). During a rhythm pause, ultrasound shows no cardiac activity but reveals a dilated RV. Pulmonary embolism is suspected—thrombolytics are administered, and return of spontaneous circulation (ROSC) follows. In this case, POCUS played a life-saving role.
Choosing the Right Protocol for the Situation
- Trauma: Go with EFAST to rule out internal bleeding or pneumothorax.
- Shock: RUSH protocol helps identify the underlying cause.
- Cardiac Arrest: Focused cardiac ultrasound to hunt for reversible problems.
- Hypotension: SHoC-ED offers a tiered approach for deeper diagnostics.
Training Makes the Difference
Mastering these protocols takes repetition—usually 25 to 50 supervised scans per type. Groups like ACEP and SCCM offer practical courses, and sim labs help build confidence. Ongoing review is key, especially since misreads (like misjudging IVC in vented patients) can lead to the wrong treatment.
Making Ultrasound Routine
To get the most from POCUS, build it into your workflow. Assign someone to scan early. Use portable machines like Kosmos for flexibility. Document findings in real-time for better transitions in care. And tackle hurdles—like time or limited devices—by streamlining how and when scans are done.
What’s Next for POCUS
The field’s evolving fast:
- AI Integration: Smarter software can now highlight signs like IVC collapse or lung barcode patterns.
- Wireless Probes: Compact and mobile, making scanning easier in tight or remote spaces.
- Tele-Ultrasound: Enables remote guidance in low-resource areas.
New uses are emerging too—like lung scans for ARDS or optic nerve sheath measurements to detect raised intracranial pressure. POCUS is becoming more central to critical care every year.
A Layered Case in Action
A 30-year-old trauma patient arrives in shock. EFAST is positive for pelvic free fluid, and surgical consultation is immediately requested. But the hypotension persists. A RUSH scan is conducted, showing a flat IVC and no tamponade—fluids are started. A lung scan is performed to exclude pneumothorax. Layer by layer, ultrasound guides management and stabilizes the patient before operation, showing how valuable and essential POCUS is.
Read more about the most important ultrasound techniques for intensivists!
Frequently Asked Questions on Ultrasound Protocols
- How sensitive is EFAST in identifying pneumothorax?
If one sees a lung point, it’s effectively 100% specific. It can be as sensitive as 50% to 90%, meaning always interpreting results in clinical context.
- What does IVC collapse signify?
If the IVC decreases by over 50% during inspiration, it usually points towards low circulating volume—hypovolemia—and is best treated with fluid administration. A distended IVC with minimal variation, however, can point towards fluid overload or obstructive etiologies like tamponade or PE.
- Can the RUSH exam be used in place of invasive monitoring?
While it doesn’t entirely replace invasive equipment, RUSH is highly useful for making expedient bedside diagnoses and can contribute to early management decisions quite effectively.
- What is the key difference between SHoC-ED and RUSH?
SHoC-ED uses a tiered, step-wise process with a focus on hypotension and cardiac arrest. RUSH uses a more broad “pump, tank, pipes” framework to assess for several shock etiologies in unstable patients.
- Is it safe to do ultrasound while CPR is in progress?
Yes—if it is done during rhythm check interruptions. If timed properly, ultrasound may yield key clues without interrupting compressions.
Conclusion
Ultrasound guidelines like EFAST, RUSH, SHoC-ED, and Cardiac Arrest Ultrasound are presently at the core of emergency and critical care. They allow doctors to quickly and precisely detect potentially life-threatening issues—e.g., pneumothorax, tamponade, or hypovolemia. They’re not just a diagnostic tool, but also dictate life-saving therapies when seconds really matter. Becoming familiar with these techniques does more than improve clinical judgment—it provides guidance and structure to the chaos of critical care.
References
- Milojevic, I., Lemma, K., & Khosla, R. (2021). Ultrasound use in the ICU for interventional pulmonology procedures. Journal of thoracic disease, 13(8), 5343–5361. https://doi.org/10.21037/jtd-19-3564
- Desai, N., & Harris, T. (2018). Extended focused assessment with sonography in trauma. BJA education, 18(2), 57–62. https://doi.org/10.1016/j.bjae.2017.10.003
- Dogan, H., & Temel, A. (2024). Diagnostic value of pulsed wave doppler in pneumothorax: a prospective study. Irish journal of medical science, 193(2), 1025–1031. https://doi.org/10.1007/s11845-023-03513-4
- Keikha, M., Salehi-Marzijarani, M., Soldoozi Nejat, R., Sheikh Motahar Vahedi, H., & Mirrezaie, S. M. (2018). Diagnostic Accuracy of Rapid Ultrasound in Shock (RUSH) Exam; A Systematic Review and Meta-analysis. Bulletin of emergency and trauma, 6(4), 271–278. https://doi.org/10.29252/beat-060402
- Furtado, S., & Reis, L. (2019). Inferior vena cava evaluation in fluid therapy decision making in intensive care: practical implications. Avaliação da veia cava inferior na decisão de fluidoterapia em cuidados intensivos: implicações práticas. Revista Brasileira de terapia intensiva, 31(2), 240–247. https://doi.org/10.5935/0103-507X.20190039
- Milne, J., Atkinson, P., Lewis, D., Fraser, J., Diegelmann, L., Olszynski, P., Stander, M., & Lamprecht, H. (2016). Sonography in Hypotension and Cardiac Arrest (SHoC): Rates of Abnormal Findings in Undifferentiated Hypotension and During Cardiac Arrest as a Basis for Consensus on a Hierarchical Point of Care Ultrasound Protocol. Cureus, 8(4), e564. https://doi.org/10.7759/cureus.564
- Ávila-Reyes, D., Acevedo-Cardona, A. O., Gómez-González, J. F., Echeverry-Piedrahita, D. R., Aguirre-Flórez, M., & Giraldo-Diaconeasa, A. (2021). Point-of-care ultrasound in cardiorespiratory arrest (POCUS-CA): narrative review article. The ultrasound journal, 13(1), 46. https://doi.org/10.1186/s13089-021-00248-0