The EchoNous Guide to Ultrasound-Guided IV Access
Ultrasound-Guided IV Access: A Modern Standard of Care
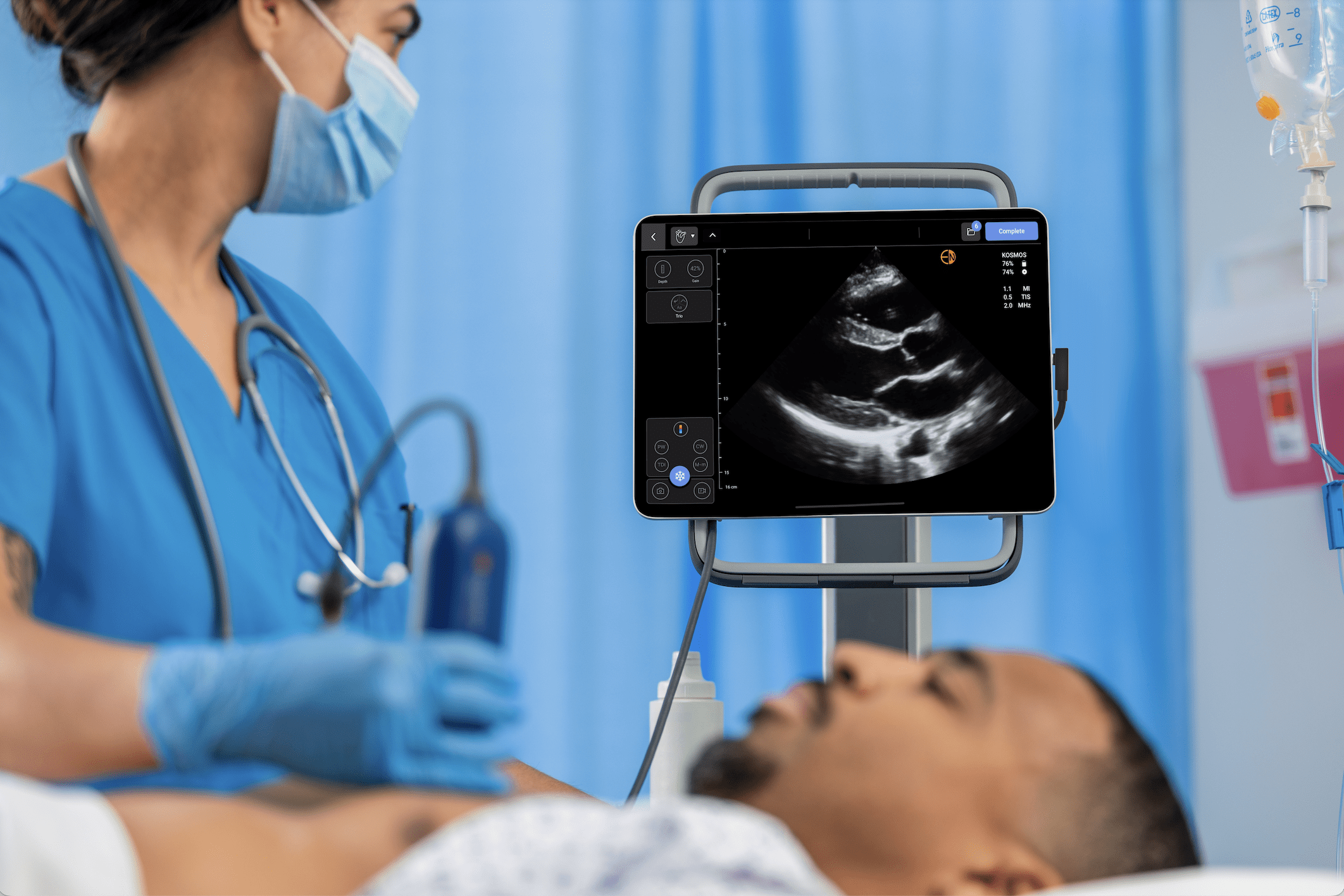
Ultrasound-guided intravenous (IV) access has emerged as a critical advance in vascular access techniques, offering a safer, more effective alternative to the traditional blind insertion method. With real-time visualization of vascular structures, clinicians can achieve higher first-attempt success rates and minimize complications, especially in patients with difficult venous access.
This article provides an overview of ultrasound-guided IV access across healthcare settings, what tools and training are required, and how it impacts clinical workflows, patient safety, and institutional costs.
Read more about the Kosmos Advantages for Vascular Access.
Table of Contents
- The EchoNous Guide to Ultrasound-Guided IV Access
- Ultrasound-Guided IV Access: A Modern Standard of Care
- Clinical Rationale for Ultrasound-Guided IV Access
- Review of Clinical Guidelines and Evidence
- Ultrasound Device Options and Probe Selection
- Training, Credentialing, and Competency Development
- Workflow Integration and Operational Efficiency [11,7]
- Patient Safety and Risk Reduction
- Cost Considerations and Return on Investment
- The Future of Ultrasound-Guided Vascular Access
- Get in Touch or Request a Demo
- References
Clinical Rationale for Ultrasound-Guided IV Access
Traditional “landmark-based” IV access relies on surface anatomy and palpation, which can be unreliable in patients with difficult venous access (DVA)—a group that includes those with obesity, chronic illness, edema, dehydration, or a history of multiple prior venous cannulations or venous sclerosis. In contrast, ultrasound guidance enables visualization of vein location, size, and depth, significantly improving outcomes.
- Fewer needle sticks and reduced patient discomfort
- Better outcomes in high-risk populations (e.g., pediatric, geriatric, oncology)
- Reduction of complications
- Avoids escalation to central venous catheterization
One study of a teaching program implemented for EM residents and ED technicians over 5 years found an 80% reduction in use of central venous catheters over the program’s life, with the largest benefit in noncritical patients[1].
Review of Clinical Guidelines and Evidence
The use of ultrasound for vascular access is supported by a growing body of clinical research and is recommended by numerous professional societies. Guidelines advocate its use in emergency departments, intensive care units, and for patients with known or anticipated DVA.
Key supporting bodies and evidence:
- Infusion Nurses Society (INS) recommends ultrasound for patients with limited venous access[2]
- The American College of Emergency Physicians (ACEP) endorses point-of-care ultrasound (POCUS) for vascular access[3]
- AIUM Practice Parameters recommend standardized use of ultrasound for vascular access[4].
Clinical trials support the use of ultrasound guidance in both adult and pediatric populations. Multiple meta-analyses confirm higher success rates and fewer complications with ultrasound compared to traditional techniques for vascular access[5,6,1].
Ultrasound Device Options and Probe Selection
Choosing the right ultrasound equipment and probe type is essential for effective IV placement. Devices range from traditional cart-based systems to compact handheld units that connect to smartphones or tablets.
Key considerations [7]:
Linear probes (high-frequency, 5–15 MHz): High resolution for superficial veins.
- Linear probes (high-frequency, 5–15 MHz): High resolution for superficial veins
- Portable and handheld units: Increasingly popular in emergency and bedside settings for mobility and ease of use
Features to look for:
- Durability
- Long battery life
- Intuitive navigation
- High level disinfection compatibility
Imaging modes:
- Basic 2D (B-mode) imaging is sufficient
- Doppler is useful to confirm vessel patency
Training, Credentialing, and Competency Development
Proper training is critical to successfully and safely use ultrasound for vascular access. Institutions should continue to develop structured training programs that combine didactic instruction with hands-on practice, simulation, and supervised clinical experience.
Training essentials:
- Fundamentals of ultrasound physics and image acquisition
- Vein identification vs. arteries and surrounding structures
- Needle visualization techniques (in-plane and out-of-plane)
- Simulation-based learning with phantoms or practice blocks • Credentialing pathways and ongoing competency assessments[8,9,10].
Workflow Integration and Operational Efficiency [11,7]
Adding ultrasound guidance to routine practice can enhance workflow efficiency, particularly in emergency or high-volume environments. It reduces time to access and often eliminates the need for more invasive procedures.
Workflow benefits:
- Faster vascular access, particularly in DVA patients
- Reduced need for central lines with their associated risks
- Empowers staff and vascular access teams
- Decreased reliance on more experienced clinicians for challenging cases
- Improved throughput in emergency departments and inpatient settings
Patient Safety and Risk Reduction
Every failed IV attempt increases the risk of complications. Ultrasound significantly enhances safety by allowing clinicians to avoid arteries, nerves, and valves and to select the most appropriate vein for cannulation.
Common complications reduced by ultrasound:
- Arterial puncture
- Hematoma and infiltration
- Infection (due to fewer attempts and shorter duration)
- Phlebitis and thrombosis
- Delays in treatment initiation
Ultrasound is especially valuable in high-risk populations where vascular access can be particularly challenging, including neonates, older people, and oncology patients.
Cost Considerations and Return on Investment
While there is an upfront cost to equipment and training, ultrasound guidance can result in significant savings over time. These savings stem from reduced complications, fewer central line placements, and improved staff efficiency.
Economic benefits:
- Lower material and labor costs from fewer repeated attempts
- Fewer escalation procedures (e.g., PICC lines or central lines)
- Shorter length of stay due to faster IV access
- Enhanced clinician productivity and reduced burnout
- Higher patient satisfaction scores and potential reimbursement gains
- Reduced economic impact from CLABSIs
One nursing study created an economic model in a large emergency department that estimated managing[12] DVA patients using traditional methods incurs an average cost of $84.29 per patient, accounting for additional insertion attempts, escalations to advanced lines, and increased clinician time. Implementing ultrasound-guided PIV access could reduce these costs by improving first-attempt success rates and reducing the need for escalated care.
In addition, the economic burden of central line-associated bloodstream infections (CLABSIs) is substantial, with average costs estimated to range from $45,000 to $90,000 per event, depending on the patient population and healthcare setting. These figures underscore the critical need for effective preventive strategies. Implementing ultrasound-guided intravenous (IV) access can significantly reduce the risk of CLABSIs by improving the success rate of peripheral IV insertions and minimizing the need for central lines, thereby mitigating these considerable financial repercussions[13].
The Future of Ultrasound-Guided Vascular Access
Innovation continues to shape the future of ultrasound in vascular access. New technologies, from AI-assisted needle guidance to integrated smart probes, make ultrasound more accessible and intuitive for frontline providers[14].
- Augmented reality (AR) and virtual simulation training tools
- Integration with electronic health records (EHRs)
- Wearable ultrasound and continuous monitoring applications
Get in Touch or Request a Demo
Ultrasound-guided IV access is a best practice supported strongly by clinical evidence, improved outcomes, and workplace efficiencies. It is no longer a niche technique. Whether you’re evaluating your first ultrasound device or scaling training across a large organization, we’re here to help. Our team at EchoNous can guide you through best practices for incorporating ultrasound for vascular access, device selection, and we can help with training & implementation solutions tailored to your needs.
Looking to add POCUS capabilities for Vascular Access to your practice? Request a Demo today.
References
- van Loon FHJ, Buise MP, Claassen JJF, Dierick-van Daele ATM, Bouwman ARA. Comparison of ultrasound guidance with palpation and direct visualisation for peripheral vein cannulation in adult patients: a systematic review and meta-analysis. Br J Anaesth. 2018;121(2):358-366. doi:10.1016/j.bja.2018.04.047
- Gorski LA, Hadaway L, Hagle ME, et al. Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs. 2021;44(1S Suppl 1):S1-S224. doi:10.1097/NAN.0000000000000396\
- American College of Emergency Physicians. Emergency Ultrasound Guidelines. Annals of Emergency Medicine. 2009;53(4):550-570.
- AIUM practice parameter for the use of ultrasound to guide vascular access procedures. (2019). Journal of Ultrasound in Medicine, 38(3). doi:10.1002/jum.14954. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/jum.14954
- Doniger SJ, Ishimine P, Fox JC, Kanegaye JT. Randomized controlled trial of ultrasound-guided peripheral intravenous catheter placement versus traditional techniques in difficult-access pediatric patients. Pediatr Emerg Care. 2009;25(3):154-159. doi:10.1097/PEC.0b013e31819a8946
- Stein, J.; George, B.; River, G.; Hebig, A.; McDermott, D. Ultrasonographically Guided Peripheral Intravenous Cannulation in Emergency Department Patients With Difficult Intravenous Access: A Randomized Trial. Ann. Emerg. Med. 2009, 54, 33–40, https://doi.org/10.1016/j.annemergmed.2008.07.048.
- Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749-757. doi:10.1056/NEJMra0909487
- Duran-hring P, Bryant L, Reynolds JA, Aldridge P, Kalynych CJ, Guirgis FW. Ultrasound-Guided Peripheral Intravenous Catheter Training Results in Physician-Level Success for Emergency Department Technicians. J Ultrasound Med. 2016;35(11):2343-2352. doi:10.7863/ultra.15.11059
- Feinsmith S, Huebinger R, Pitts M, Baran E, Haas S. Outcomes of a Simplified Ultrasound-Guided Intravenous Training Course for Emergency Nurses. J Emerg Nurs. 2018;44(2):169-175.e2. doi:10.1016/j.jen.2017.10.001
- Hoskins, Michael J. MD, MHPEd, BSca,b,*; Nolan, Brieana C. MD, MHPEd, BSca,b; Evans, Kiah L. PhD, GradCert(ResComm), GradCert(HPE), BSc(OT)Honsa; Phillips, Bríd PhD, MA(Dist), GradCert(TerTeach), FHEAc. Educating health professionals in ultrasound guided peripheral intravenous cannulation: A systematic review of teaching methods, competence assessment, and patient outcomes. Medicine 102(16):p e33624, April 21, 2023. | DOI: 10.1097/MD.0000000000033624
- Stuckey C, Curtis MP. Development of a nurse-led ultrasound-guided peripheral intravenous program. J Vasc Nurs. 2019;37(4):246-249. doi:10.1016/j.jvn.2019.07.003
- Gala S, Alsbrooks K, Bahl A, Wimmer M. The economic burden of difficult intravenous access in the emergency department from a United States’ provider perspective. J Res Nurs. 2024;29(1):6-18. doi:10.1177/17449871231213025
- Zimlichman, E., et al. (2013). Impact of healthcare-associated infections on length of stay and costs in hospitalized patients. Infection Control & Hospital Epidemiology, 34(10), 1039-1046.
- Panebianco, N.L.; Fredette, J.M.; Szyld, D.; Sagalyn, E.B.; Pines, J.M.; Dean, A.J. What You See (Sonographically) Is What You Get: Vein and Patient Characteristics Associated With Successful Ultrasound‐guided Peripheral Intravenous Placement in Patients With Difficult Access. Acad. Emerg. Med. 2009, 16, 1298–1303, https://doi.org/10.1111/j.1553-2712.2009.00520.x
Additional References
Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. AHRQ Publication No. 08-0043. Rockville, MD: Agency for Healthcare Research and Quality; 2008. https://pubmed.ncbi.nlm.nih.gov/21328752
Moore CL. Ultrasound first, second, and last for vascular access. J Ultrasound Med. 2014;33(7):1135-1142. doi:10.7863/ultra.33.7.1135
Peralta-Gámez MS, Gómez de Quero Córdoba M, Reverté-Villarroya S, Cuesta-Martínez R. Comparison of Traditional and Ultrasound-Guided Techniques for Vascular Access in Patients with Difficult Venous Access in Emergency Departments: Randomized Clinical Trial Protocol. Nursing Reports. 2025; 15(5):177.
Stokowski, G.B.; Steele, D.R.; Wilson, D.P. The Use of Ultrasound to Improve Practice and Reduce Complication Rates in Peripherally Inserted Central Catheter Insertions. J. Infus. Nurs. 2009, 32, 145–155, https://doi.org/10.1097/nan.0b013e3181a1a98f.