Dr. Josè Pinto: A Surgeon’s Perspective on the Evolution of POCUS and Trauma Assessment
Point-of-Care Ultrasound (POCUS) is rapidly transforming modern medicine, moving from a specialized tool to becoming a key part of everyday clinical practice. Dr. Josè Pinto, a general surgeon from Porto, Portugal, has been a proponent of POCUS since its early days. Dr. Pinto emphasizes that ultrasound should be considered the “fifth pillar” of the physical examination, alongside inspection, auscultation, palpation, and percussion. He believes that a patient examination is incomplete without POCUS. The EchoNous team recently spoke with Dr. Pinto about his career in medicine and his vision for the future of POCUS.
Table of Contents
The Evolution of the EFAST Exam
Dr. Pinto’s journey with ultrasound began during his residency in Braga, Portugal, where he was first introduced to the EFAST (Extended Focused Assessment with Sonography in Trauma) protocol. He quickly recognized its potential to revolutionize trauma care. The EFAST exam, a widely studied POCUS protocol, has evolved significantly since its origins in the 1970s.
Starting as the FAST exam (Focused Abdominal Sonography in Trauma), the protocol focused on assessing the abdominal cavity for free fluid in three areas: the right hypochondrium, left hypochondrium, and suprapubic space. This non-invasive approach was a significant improvement over the traditional diagnostic peritoneal lavage (DPL), which involved a mini-laparotomy and carried risks of false positives and unnecessary surgeries. As Dr. Pinto explains, DPL often led to “blank laparotomies” where no surgical lesion was found, resulting in a more aggressive and unneeded intervention for the patient.
In the 1990s, with the ATLS (Advanced Trauma Life Support) guidelines, FAST evolved to include an assessment of the pericardium for cardiac tamponade, becoming “Focused Assessment Sonography in Trauma”. This expansion allowed for rapid detection of life-threatening cardiac conditions in trauma patients. By the early 2000s, the protocol further expanded to include thoracic evaluation for hemothorax and pneumothorax, leading to the “Extended FAST” (EFAST) exam as it is known today.
The EFAST protocol allows clinicians to quickly identify free fluid or air in the chest and abdomen, and fluid in the pericardial area within three to five minutes. Dr. Pinto highlights that even with limited experience (20-30 exams), clinicians can become proficient in identifying abnormalities, making it an invaluable tool for guiding immediate decisions in trauma settings.
The Unquestionable Advantages of POCUS
Dr. Pinto champions POCUS for its numerous advantages, particularly in trauma and surgical contexts. POCUS is:
- Non-invasive: Unlike DPL or even CT scans, it doesn’t involve surgical incisions or radiation exposure
- Quick and Dynamic: It provides real-time information, enabling rapid decision-making at the bedside. This immediacy is crucial in emergency situations where “time is of the essence”
- Repeatable: It can be performed as many times as needed without any adverse effects on the patient
- Cost-effective: When machines and know-how are available, it offers a more economical solution compared to traditional imaging
Dr. Pinto emphasizes that POCUS empowers clinicians to make decisions quickly and with confidence. He recalls a medical school teacher who taught that surgeons should “see with their fingertips,” but with ultrasound, he can “see beyond” what his hands can perceive. This ability to visualize internal structures provides a profound sense of confidence, allowing surgeons to make informed decisions about intervention or conservative management. This is particularly beneficial for stable patients with important trauma mechanisms, where an EFAST exam can reveal subtle abnormalities that might otherwise be missed, guiding further tailored approaches.
Overcoming Barriers to POCUS Adoption
Despite the clear benefits, widespread adoption of POCUS still faces significant hurdles. Dr. Pinto identifies several key barriers:
- Mindset and Resistance to Change: Many healthcare professionals are comfortable with existing practices, such as relying on CT scans and radiologist reports, and are hesitant to adopt new technologies. This can sometimes stem from a “defensive medicine” approach, where clinicians prefer to operate behind the “wall” of a formal radiology report. However, Dr. Pinto argues that not using readily available ultrasound machines can also expose clinicians to accountability risks if a life-threatening condition is missed.
- Lack of Education and Training: A significant barrier is the perceived complexity of learning ultrasound. Clinicians need to recognize that ultrasound machines are simply tools, akin to a stethoscope, and that proficiency doesn’t require a PhD in physics. Dr. Pinto highlights the importance of early exposure in medical schools and continuous learning through courses and mentorship.
- Staffing and Resources: Insufficient trained personnel and a lack of established institutional protocols can hinder POCUS integration into daily workflows. Dr. Pinto notes that busy emergency departments with short-staffed surgical teams may find it challenging to allocate time for POCUS exams.
- Need for a Supportive Community: Dr. Pinto stresses the importance of a POCUS community for ongoing skill refinement, sharing experiences, and learning from peers. He advocates for sharing case reports and videos, even through informal channels like WhatsApp, to foster this collaborative learning environment.
Dr. Pinto is actively involved with POCUSX, an independent company that provides POCUS education, where he coordinates the EFAST course. He is encouraged by the increasing inclusion of EFAST in ATLS re-certification courses, seeing it as a sign of progress. He urges trauma professionals to be “missionaries” in spreading the word about POCUS, emphasizing that it can make clinicians more comfortable in stressful trauma situations
The Role of AI in POCUS and the Future of the Physical Exam
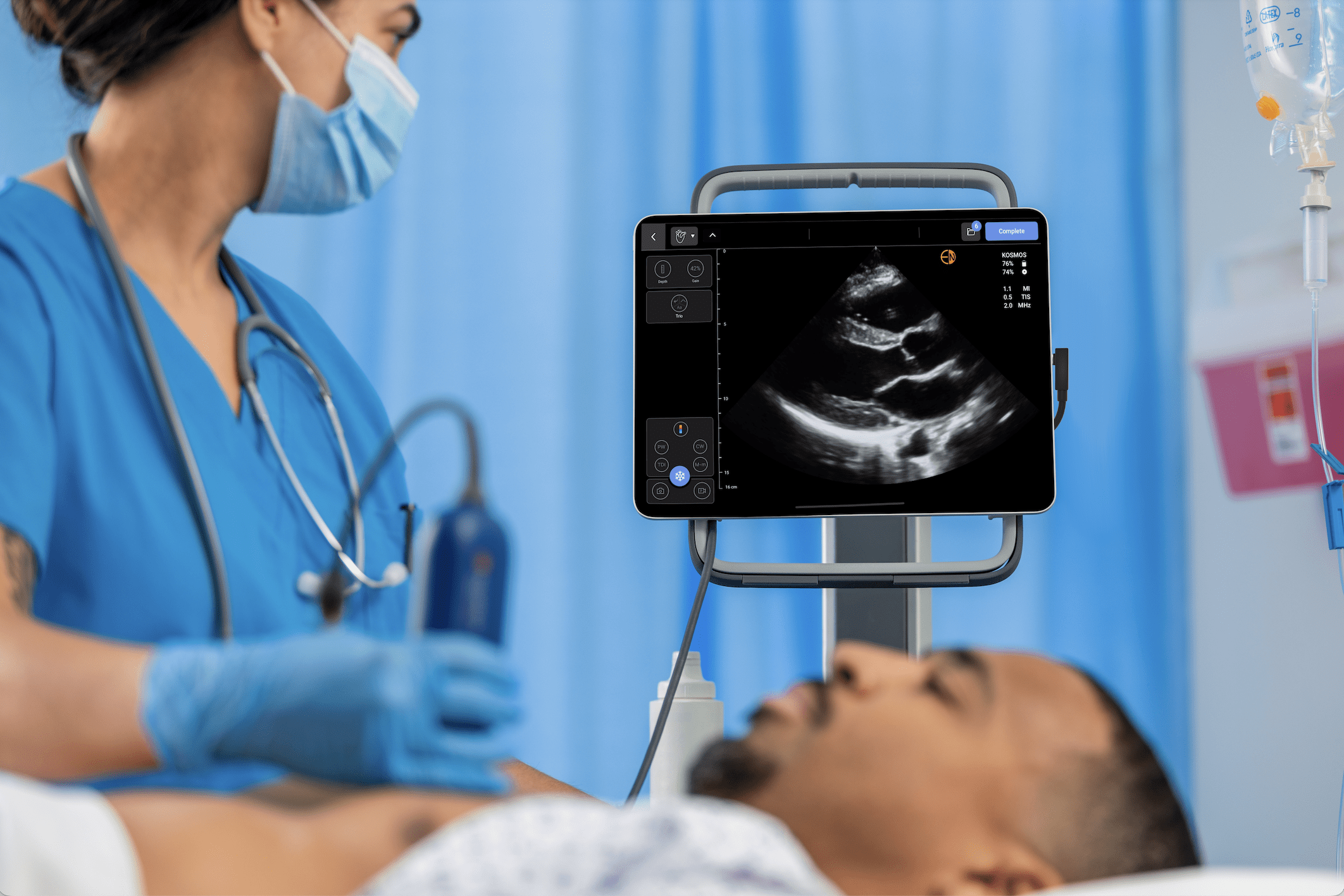
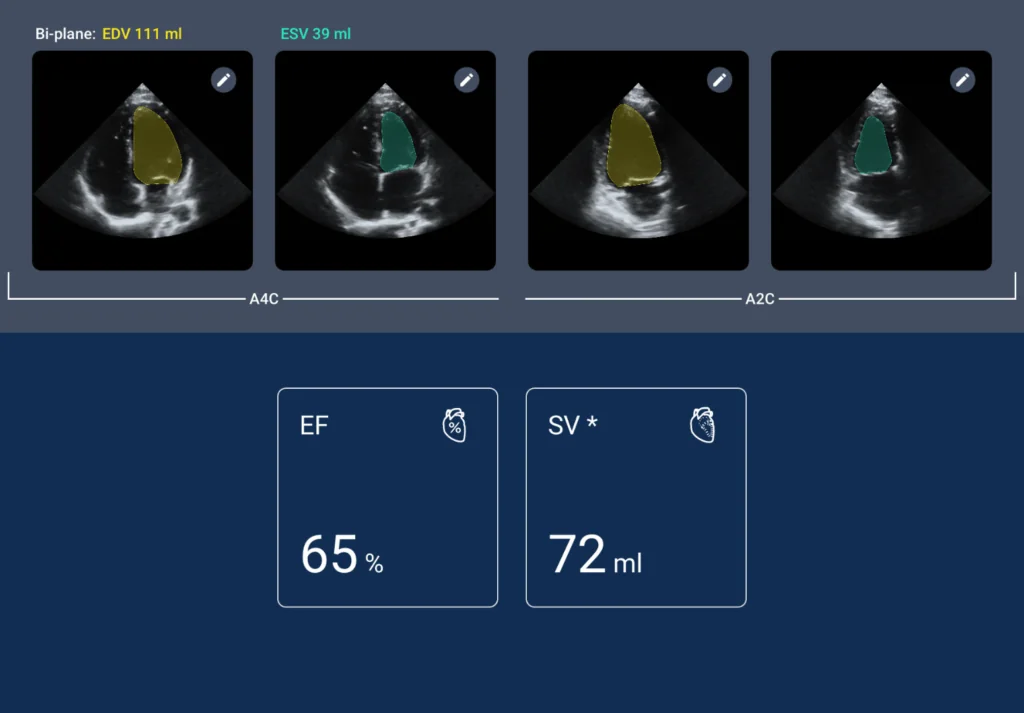
Dr. Pinto acknowledges the transformative potential of AI in ultrasound. He has experience using devices like the Kosmos ultrasound system with AI software, noting its utility in teaching settings. The AI features, such as automated anatomical labeling, are particularly beneficial for new users, helping them by confirming their interpretations of the on-screen anatomy. This aligns with EchoNous’s goal of making ultrasound easier to learn and more efficient for both new and experienced users.
POCUS, he envisions, will become as ubiquitous as the stethoscope in the future. He believes that medical students are increasingly being exposed to POCUS early in their training, and future generations of clinicians will naturally expect it to be an integral part of their practice.
For Dr. Pinto, ultrasound is not just an adjunct but a fundamental part of a complete physical examination. It allows clinicians to “see things, not what you can suppose,” providing objective information that enhances diagnostic accuracy and patient care. He argues that without ultrasound, a medical examination is incomplete.
Kosmos – Empowering the Fifth Pillar of the Physical Exam
The Kosmos ultrasound system by EchoNous stands at the forefront of this revolution, directly addressing the needs and challenges highlighted by Dr. Pinto. With its advanced AI capabilities, Kosmos is designed to help flatten the learning curve for new users, offering features like AI anatomic labeling that provides real-time confidence during scans. This not only aids in accelerating proficiency but also reinforces accurate interpretation, making the transition to routine POCUS use more seamless for clinicians across specialties.
By combining high-quality imaging with intuitive AI assistance, Kosmos can be an indispensable “fifth pillar” of the physical examination.
To learn more, connect with a clinical product expert or request a personalized demo today.