Enhancing the Foundation:
Dr. Steelman’s Direct Primary Care Model with POCUS
Dr. William Steelman
DO, FACOI
Dr. William Steelman, DO, FACOI, and founder of Steelman Medical Group, recently discussed the impact of point-of-care ultrasound (POCUS) technology on primary care with Luke Baldwin, VP of Global Marketing at EchoNous.
After 12 years of medical practice, he fulfilled his long-held aspiration by establishing Steelman Medical Group, a primary care organization focused solely on meeting patients’ needs without bureaucratic hindrances.
Meet Dr. William Steelman
Dr. William Steelman, DO, FACOI, was born in Virginia Beach and grew up in a US Navy family, moving frequently along the East Coast before settling in Ocean Springs, Mississippi. He earned a BS in Chemistry from Millsaps College in Jackson, Mississippi, followed by graduate studies in Pharmacology and Toxicology. Dr. Steelman then attended osteopathic medical school at Kansas City University of Medicine and Biosciences.
After 12 years of medical practice, he fulfilled his long-held aspiration by establishing Steelman Medical Group, a primary care organization focused solely on meeting patients’ needs without bureaucratic hindrances.
Dr. Steelman’s Journey to DPC
Dr. Steelman’s medical journey has been a testament to adaptability, spanning over a dozen hospitals along the East Coast, where he honed his skills across various specialties. A commitment to learning and a passion for patient care has defined Dr. Steelman’s journey from emergency rooms to primary care clinics.
Through locum tenens moonlighting, Dr. Steelman gained exposure to diverse medical environments, sharpening his diagnostic and patient care abilities along the way. This hands-on experience in real-world settings led him to a key insight: there was a more effective model for patient care than the traditional healthcare system.
That’s why Dr. Steelman embraced the concept of direct primary care (DPC) to provide more personalized and accessible healthcare to his patients. In DPC, he found the freedom to focus on patient relationships and comprehensive care without the constraints of insurance bureaucracy.
Dr. Steelman explains, “Being independent means that I can also set healthcare plans and goals for patients that otherwise would be ignored. The access to care really changes lives, and that’s huge.”
By limiting his patient census and eliminating insurance barriers, Dr. Steelman can offer more extended appointment times and thorough examinations, ensuring that each patient receives the attention they deserve. This patient-centric approach aligns with his vision of a healthcare model that prioritizes individual needs over administrative demands.
At the same time, Dr. Steelman has also embraced innovation, integrating technology into his practice to enhance patient care and streamline medical processes. From handheld ultrasound devices to artificial intelligence (AI) diagnostics, he leverages cutting-edge tools to improve diagnostic accuracy and treatment outcomes.
“Essentially, [technology] is saving us time and allowing us to place that resource back into patient care. As doctors, that is what we have always wanted.”
By harnessing the power of AI for preliminary readings and utilizing portable ultrasound devices for on-the-go diagnostics, Dr. Steelman can provide more timely and accurate assessments.
Beyond diagnosis and treatment, Dr. Steelman is committed to empowering his patients through education and preventive care. Recognizing the importance of lifestyle modifications in managing chronic conditions, he emphasizes the role of nutrition, exercise, and stress management in promoting overall well-being.
Dr. Steelman emphasizes the significance of preventive care: “Avoiding the standard American diet of processed foods and added sugar is about 80% of the battle, so if I just start there and stick to that, I won’t lose a lot of people.”
Through continuous monitoring and personalized healthcare plans, Dr. Steelman equips his patients with the knowledge and tools necessary to take control of their health. By fostering a collaborative relationship, he ensures patients are actively involved in their healthcare decisions, leading to better long-term outcomes.
Today, Dr. Steelman heads Steelman Medical Group, a healthcare organization focused on personalized healthcare and community-focused medicine. As the founder and lead physician, he embodies the principles of direct primary care, prioritizing patient relationships and comprehensive patient care.
Establishing his practice was a natural progression for Dr. Steelman, who sought to create a healthcare environment where patients felt valued and heard. Unlike traditional primary care practices, where physicians may see upwards of 20 patients a day, Dr. Steelman caps his panel size to prioritize quality over quantity.
“We see a limited panel… on average, [in] the family practice world, about 1% of your panel will come through your door every day. So, capping at 600 puts me at about six interactions a day, which is about average.”
By maintaining a smaller patient panel, Dr. Steelman can offer extended appointment times, more thorough examinations, and personalized care plans tailored to each patient. This approach fosters stronger doctor-patient relationships and allows for more in-depth discussions about preventive measures and lifestyle modifications.
As a community doctor, Dr. Steelman plays an integral role in the lives of his patients, providing continuity of care and serving as a trusted healthcare advocate. In founding his practice, he has realized his vision for a more patient-centered healthcare model and has become a driving force for positive change in the medical community.
The Direct Primary Care Model
Central to the philosophy of Dr. Steelman’s practice is Direct Primary Care (DPC), a new approach to healthcare delivery that prioritizes accessibility, affordability, and quality.
Direct Primary Care, as championed by Dr. Steelman and his team, is a membership-based model that removes the barriers often associated with traditional healthcare systems. In a DPC practice, patients pay a monthly or yearly fee in exchange for comprehensive primary care services, eliminating the need for insurance intermediaries and copays.
“In direct primary care, we see a limited panel,” Dr. Steelman explained. “We don’t charge for copays, return visits, and things like that.”
By operating outside the confines of insurance-based reimbursement models, DPC practices like Steelman Medical Group can focus on what truly matters: delivering high-quality, personalized care without the bureaucratic constraints often imposed by third-party payers.
This shift towards a membership-based model not only enhances the doctor-patient relationship but also empowers patients to take an active role in their healthcare journey. With easier access to their primary care physician, patients can seek medical advice, schedule appointments, and address concerns promptly and conveniently.
Furthermore, DPC practices like Steelman Medical Group embrace a holistic approach to healthcare, emphasizing preventive care, wellness initiatives, and chronic disease management. By prioritizing early intervention and proactive health measures, DPC physicians can help patients achieve optimal health outcomes and reduce the reliance on costly interventions down the line.
In this way, Dr. Steelman’s work echoes that of Dr. Peter Fitzgerald, who underscored the importance of “bending of the curve” before health issues manifest and advocates for strategies that foster healthy lifestyle choices and engage patients from the start.
Direct Primary Care represents a paradigm shift in the healthcare landscape, placing the patient at the center of the equation and redefining the doctor-patient relationship.
Traditionally, primary care has been synonymous with insurance-based reimbursement models, copays, and administrative overhead. Patients navigate a labyrinth of paperwork and bureaucracy, often with limited appointment availability and rushed consultations.
“The biggest problem with being a physician in modern-day life is knowing that you can do better and not being able to do it,” Dr. Steelman said.
Enter Direct Primary Care—a game-changing alternative to traditional primary care. DPC reimagines healthcare delivery at its core by forging a direct relationship between patients and physicians, unencumbered by the constraints of insurance intermediaries.
This shift towards a membership-centric approach affords numerous benefits for both patients and physicians. Patients enjoy easier access to their primary care provider, extended appointment times, same-day or next-day visits, and enhanced continuity of care. Meanwhile, physicians like Dr. Steelman can prioritize quality over quantity, fostering deeper connections with patients and delivering personalized, evidence-based care without the administrative burdens imposed by insurance companies.
In essence, Direct Primary Care represents a departure from the status quo characterized by accessibility, affordability, and patient-centeredness. Dr. Steelman notes, “This system allows me to operate outside of [the insurance-based model], and [patients] can still bill their insurance for procedures and imaging things… It’s triple tax preferred. It’s fantastic.”
Unlike fee-for-service models, DPC operates on a transparent, fixed-fee structure, providing patients with financial predictability. This straightforward pricing model alleviates financial strain, enabling patients to prioritize their health without worrying about unexpected expenses.
DPC also fosters extended patient-physician interactions, promoting trust and collaboration. Dr. Steelman notes, “If I spend an hour with you now and then, in three months, we can catch up again…we’re really changing the game in terms of outcomes.” This emphasis on preventative care and proactive management improves patient outcomes and cultivates a culture of wellness.
Use of POCUS in his practice
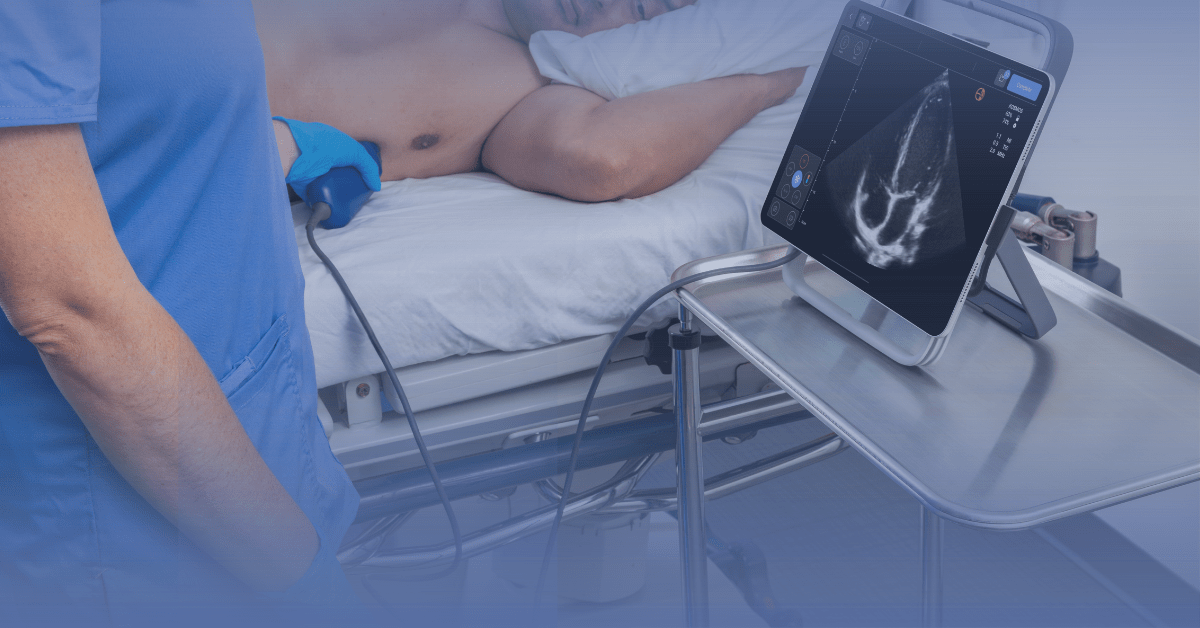
Dr. Steelman has long recognized the transformative potential of ultrasound in enhancing diagnostic capabilities and improving patient care within his practice. Having experienced the limitations of traditional healthcare settings, he sought to integrate innovative technologies to optimize clinical outcomes, including point-of-care ultrasound (POCUS).
“Having this kind of tool and the ability to pull something out of my bag that lets me get a confirmatory diagnosis or track someone who needs this kind of thing really makes a big difference,” he said.
By leveraging ultrasound technology, Dr. Steelman aims to expedite diagnostic processes, facilitate informed decision-making, and empower patients with timely, accurate medical insights.
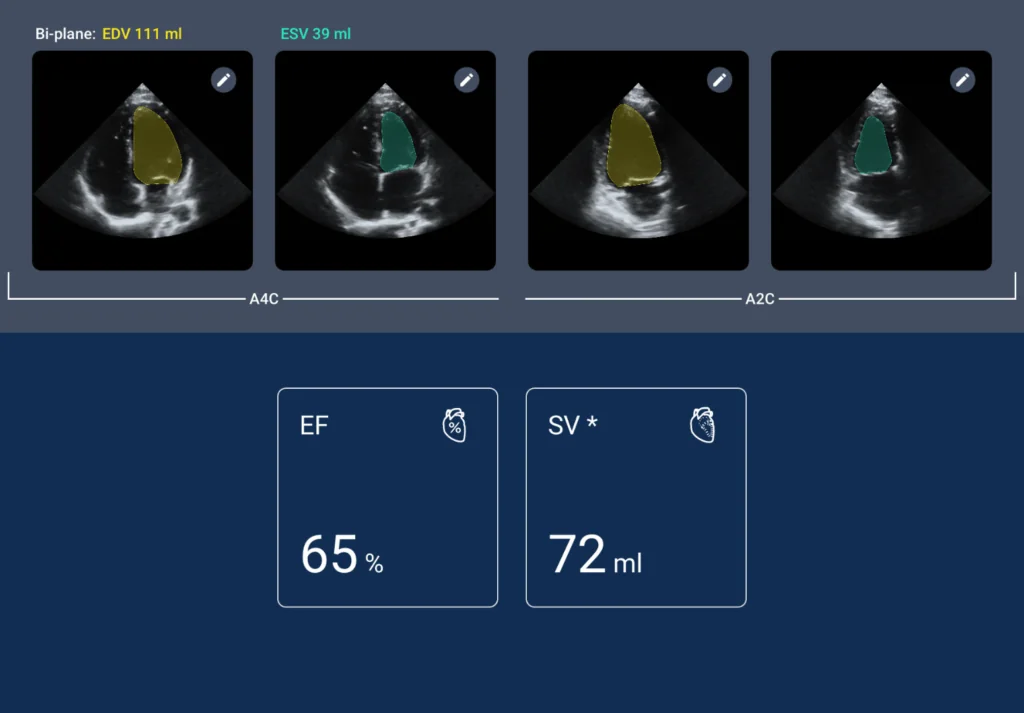
In his practice, Dr. Steelman employs ultrasound as a versatile diagnostic tool to enhance patient care across various medical contexts. Whether assessing cardiac function, detecting joint abnormalities, or guiding procedural interventions, ultrasound enables precise, real-time visualization, empowering Dr. Steelman to deliver personalized, evidence-based care to his patients.
Dr. Steelman’s patients have responded positively to integrating ultrasound into their healthcare experience. “In terms of how people interact with it – they love it. They love having a doctor who is ahead of the curve or following along,” he said.
This sentiment underscores the patient-centered nature of Dr. Steelman’s practice, where the adoption of advanced technology fosters trust and confidence in medical care. By leveraging ultrasound as a diagnostic adjunct, Dr. Steelman enhances patient engagement and satisfaction while promoting a collaborative approach to healthcare management.
The impact of POCUS on diagnosing and managing health conditions more efficiently and cost-effectively is profound. POCUS streamlines the diagnostic process by eliminating the need for referrals to imaging centers or hospitals, reducing wait times and alleviating patient anxiety. Dr. Steelman’s proactive approach to healthcare, enabled by POCUS, allows for early detection of abnormalities and prompt initiation of treatment, ultimately improving patient satisfaction and adherence to care plans.
Furthermore, by integrating POCUS into his practice, Dr. Steelman minimizes healthcare costs for his patients. With on-site ultrasound capabilities, patients can avoid unnecessary referrals and imaging expenses, resulting in significant cost savings. Dr. Steelman emphasizes the value of POCUS in delivering high-quality, cost-effective care.
“It’s an easy return on investment because I can use it to directly provide care to my patients and save them money,” he said.
Growth of Direct Primary Care
The Direct Primary Care (DPC) model, championed by Dr. Steelman, emerges as a potential remedy to the challenges of the current healthcare paradigm. With its emphasis on patient-centered care, accessibility, and affordability, DPC holds promise in addressing the systemic issues facing traditional healthcare systems.
“I believe this model is changing,” Steelman said. “When people see that direct primary care physicians can do medicine the way that we’re trained, the way we want to provide medicine and the way patients want it, it makes a lot more sense.”
Moreover, the DPC model offers intrinsic incentives for physicians, particularly those considering specialization in Family and Internal Medicine. For example, Dr. Steelman underscores the financial advantages associated with DPC.
“They say it’s about a 30% increase in physician pay because it’s cash-based,” he notes. “Being independent means that I can also set healthcare plans and goals for patients that otherwise would be ignored.” This suggests that DPC could attract more doctors to these specialties by offering greater autonomy and financial rewards.
Dr. Steelman’s approach to healthcare, characterized by personalized patient relationships and accessibility, serves as a compelling case study in contemporary medical practice. By prioritizing direct interaction and leveraging technology to enhance accessibility, Dr. Steelman demonstrates a patient-centric approach that resonates with the evolving expectations of healthcare consumers.
His emphasis on personal relationships and open communication with patients reflects a departure from the traditional, transactional healthcare delivery model. Dr. Steelman’s integration of modern communication tools, such as electronic medical records and telemedicine platforms, facilitates seamless patient-physician interaction beyond the confines of the clinical setting.
“Patients today expect more from their doctors,” he said. “They see things they’ve read online and text me, seeking advice and asking if they should be worried, and I have to be prepared to answer it.”
In essence, Dr. Steelman’s approach exemplifies the potential of personalized, technology-enabled healthcare delivery to meet the needs and preferences of today’s patients. As the healthcare landscape evolves, his story is a testament to the transformative impact of patient-centered care and modern technology in driving positive health outcomes.
“Having this kind of tool and the ability to pull something out of my bag that lets me get a confirmatory diagnosis or track someone who needs this kind of thing really makes a big difference,” he said.
By leveraging ultrasound technology, Dr. Steelman aims to expedite diagnostic processes, facilitate informed decision-making, and empower patients with timely, accurate medical insights.
In his practice, Dr. Steelman employs ultrasound as a versatile diagnostic tool to enhance patient care across various medical contexts. Whether assessing cardiac function, detecting joint abnormalities, or guiding procedural interventions, ultrasound enables precise, real-time visualization, empowering Dr. Steelman to deliver personalized, evidence-based care to his patients.
Dr. Steelman’s patients have responded positively to integrating ultrasound into their healthcare experience. “In terms of how people interact with it – they love it. They love having a doctor who is ahead of the curve or following along,” he said.
This sentiment underscores the patient-centered nature of Dr. Steelman’s practice, where the adoption of advanced technology fosters trust and confidence in medical care. By leveraging ultrasound as a diagnostic adjunct, Dr. Steelman enhances patient engagement and satisfaction while promoting a collaborative approach to healthcare management.
The impact of POCUS on diagnosing and managing health conditions more efficiently and cost-effectively is profound. POCUS streamlines the diagnostic process by eliminating the need for referrals to imaging centers or hospitals, reducing wait times and alleviating patient anxiety. Dr. Steelman’s proactive approach to healthcare, enabled by POCUS, allows for early detection of abnormalities and prompt initiation of treatment, ultimately improving patient satisfaction and adherence to care plans.
Furthermore, by integrating POCUS into his practice, Dr. Steelman minimizes healthcare costs for his patients. With on-site ultrasound capabilities, patients can avoid unnecessary referrals and imaging expenses, resulting in significant cost savings. Dr. Steelman emphasizes the value of POCUS in delivering high-quality, cost-effective care.
“It’s an easy return on investment because I can use it to directly provide care to my patients and save them money,” he said.
Stay posted for upcoming Q&A article, where Dr. Steelman dives deeper into his innovative approach to healthcare, the transformative impact of Direct Primary Care (DPC), and the integration of cutting-edge technology like point-of-care ultrasound (POCUS) into his practice.
To learn more about Kosmos, contact us today!