10 Steps to Developing a Medical School Ultrasound Program
Developing a new or existing ultrasound program for a medical school can feel daunting. So we spoke to three prominent ultrasound educators – Dr. David Bahner, Dr. Wilma Chan, and Dr. Richard Hoppmann to outline the 10 critical steps to consider when developing your ultrasound education program.
The following is an edited transcript of the doctor’s interviews. You can view a video of the interviews here.
1. What are the factors to consider when involving stakeholders for launching an ultrasound program?
Dr. Richard Hoppmann: Thinking about the stakeholders involved in the curriculum, we need to look at a vast spectrum. Everything from the medical students, all the way up to the Dean. Critical stakeholders are course directors, clerkship directors, and those involved in content. Also, identify a subgroup of champions because you need champions in the very beginning.
One way to involve stakeholders could be to send out an announcement of the idea of starting an ultrasound curriculum and see what response you get from it. Then, meet with those individuals and get a sense of what they think about ultrasound and what they think their role may be – if you can get a champion across several courses and clerkships, I think that puts you in a very good position. Get your whole group together and get a sense of how interested stakeholders are in moving forward with this, and you can also get a sense of what role they want to play.
I think the same thing would be true with the medical students. Medical students can be a driving force in getting an ultrasound curriculum going. One of the things that we did early on was to send out a similar sort of announcement and say, we’re looking at this, we want your input, we want you to feel ownership in this because it does belong to the medical students. The next step would be to get those leaders among the medical students and form an interest group. The interest group can be very important in terms of feedback, and they can help teach as well. Identifying the stakeholders, bringing stakeholders together, and having everybody feel like they are a part of this program is very important.
2. What are the factors to consider when securing financial support when launching an ultrasound program?
Dr. David Bahner: When you’re starting an ultrasound medical education program, the budget and funding are some of the most challenging questions to answer. The first thing you need to answer is, do you have your own time to try to put into these efforts, because your time is not always going to be compensated hour for hour.
Trying to find funding is a matter of talking to your direct reports, your chairs to see if there are ways that your department can help fund these efforts into medical education. You can try to talk with your medical school to see if some of the efforts and skill sets you have are consistent with what they are trying to teach the students and find funding from the college of medicine. You can try to write research grants and educational grants, but those are a little bit harder. There are different programs within the industry, but I think that when you’re trying to budget for funding, it’s essential that this is something you have the time to try to overcome because the budgetary issues are complex. There’s a lot of time on the front end that you have to put in, where there is no funding, but as you progress and have a product, you can work with the medical school, your department, or the industry.
It’s a different landscape than 20 years ago because there’s been a lot more literature produced. There’s a lot more momentum, and the ultrasound machines have gotten a lot smaller. So, ultrasound in medical education is not as big of a stretch as it was perhaps in 1999 when I started. Perseverance and allocating time to put in your budget does pay off in the end. When you’re trying to find funding, it’s crucial to develop that budget, work with your department, and then work with the college to find support for the things you’re teaching that goes along with their curricula.
3. What are the factors to consider when recruiting experts to teach ultrasound?
Dr. Wilma Chan: The challenge of getting the right experts to teach ultrasound – it has been, and probably will always be, a huge battle. In the very beginning, we were scrambling around to get experts. Our experts were anyone willing to teach a couple of medical students with the machines we had, with topics they were comfortable with, so we were certainly flexible around who was teaching our students, and we got a lot of feedback from students.
I don’t think that the skill of teaching correlates with years of experience. There’s a certain skill set that comes with bedside teaching that is based on how comfortable the learner is with the instructor. A lot of what we’ve experienced recently is that our expert teachers are near-peer instructors. So, we have many senior medical students who are now teaching our students. They are nowhere close to expert level in terms of the content, but they have learned a certain script and understand the philosophy of how we teach ultrasound. They have gone on to be excellent ambassadors and stewards of ultrasound, so we have required less faculty and senior-level involvement.
We also have a sonographer educator. She has had decades of experience with the radiology departments doing ultrasound as a technician, and she has been invaluable in the way we deliver ultrasound education. She is there as technical support, equipment support, and someone to bounce ideas off for curriculum and content development.
4. What are the factors to consider when designing/curating content to teach ultrasound?
Dr. Wilma Chan: The challenge of deciding what content to share with your students and what to use as preparation materials will be probably a topic of debate among many people. Some people are purists and want to develop all their content independently. Sometimes that’s not based on the instructor’s decision or the course director’s decision. Sometimes schools mandate a certain feel or a format of how their content is put up on whatever forum that they’re on – eg. Blackboard.
That part is unfortunate because there’s so much good content out there that has been done and redone and edited. My philosophy is that you don’t need to reinvent the wheel. There’s a lot of great content out there. As the instructor and director of a course, you can review this content and make sure it is appropriate for your level of learner, and the length of the content is suitable for the learner’s attention span.
The scope of topics is so broad that I think people tend to become overwhelmed. For anyone who’s starting off, choose less than a handful of topics that you think are important and vital to your institution and stick with it. Just because someone else at a different institution teaches 16 topics doesn’t mean you need to go with 16 topics. You can teach four topics well and make sure that the content is very well curated and updated often to ensure its quality. So that would be my recommendation – keep it narrow and focused, prioritize what your institution needs to deliver, and don’t reinvent the wheel.
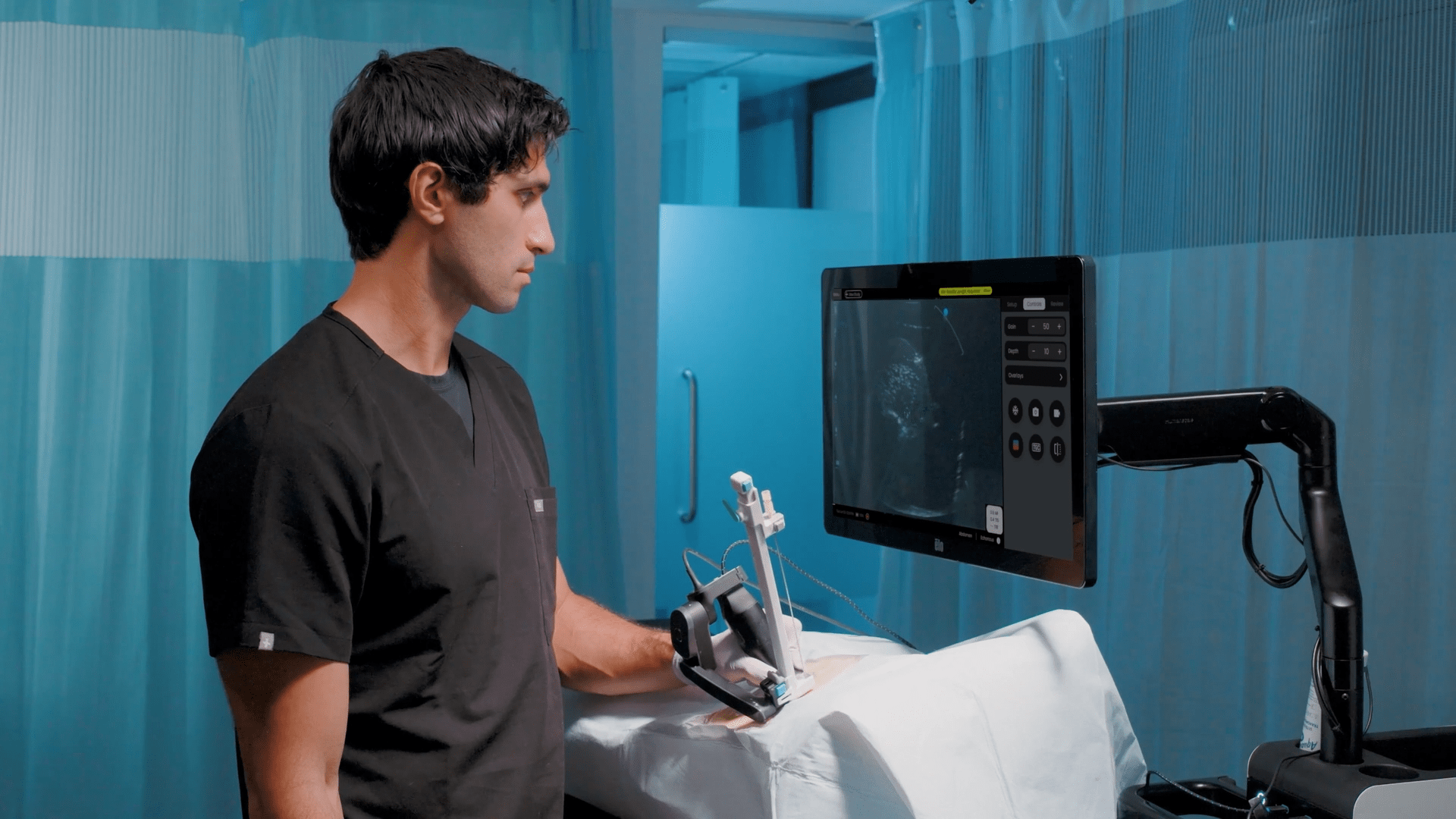
5. What are the factors to consider when selecting devices to teach ultrasound?
Dr. Richard Hoppmann: In the United States, the average class size is about 165 students, but the range is less than a hundred to over 300. So, you need to look at your class size and how extensive the curriculums will be.
Is it going to be a basic introductory class or a more comprehensive class in which you’ll need more devices? I guess the bottom line would be that the more devices, the better, but obviously, you have to fit that into your budget. I think in terms of devices, look at your class size and see what you want to do. The advantages of a single device make it easy and efficient because everybody knows that device. Some feel more comfortable helping if they know they held the machine they could be using, so they’re more inclined to participate. However, there’ll be some limitations in terms of the labs that you can do.
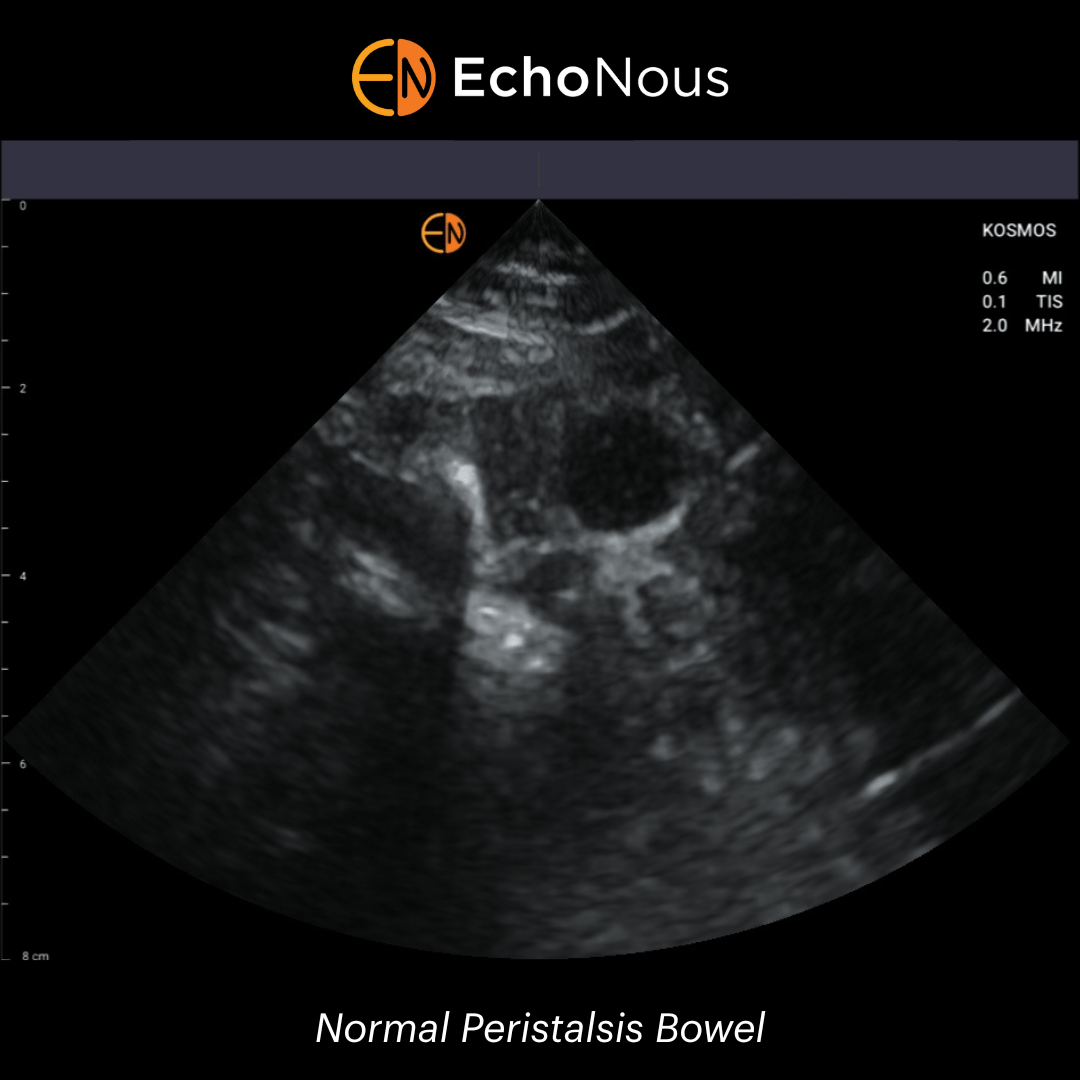
In terms of multiple devices, you get a broader experience. And then the final part is AI. AI will play a significant role in medicine, especially in education. I think anytime you can get devices that allow self-directed learning, such as with real-time labeling of anatomy, the direction of probe manipulation, image quality, all those things will help because the key will be how much instruction you can turn over to the self-learner.
6. What are the factors to consider when requesting time to teach ultrasound?
Dr. Richard Hoppmann: The curriculum has been an issue from the very beginning. I think the key to that is what value it brings to teaching. One approach is to start small. Make sure you don’t overwhelm students or faculty. You gain some successes, get good feedback, and then you can expand. I suggest spreading things out instead of packing most of your ultrasound into one or two courses and one or two clerkships. If you spread it out across the curriculum, then you only have to ask for a little bit of time in each course, in each clerkship. And then usually people can tolerate that, and it expands. As the student feedback comes in, the faculty asks if more can be done. Start small, make sure it goes well, and build from that. And then things will go well after that.
7. What are the factors to consider when assessing competency while teaching ultrasound?
Dr. David Bahner: Assessment drives learning, so it’s essential to focus on assessment. Whenever you’re trying to start a medical school ultrasound program, there must be a clear objective and clear curriculum. We have some local curriculum versions with our learning management system. We have some local ways that the students will track the number of exams they have. You can work with industry, having other tools to try to help you follow some of the various ways people are saving scans and having those images reviewed.
We have a series of courses that we have put together, and one of the best ways we assess is with an oral exam, where they present their portfolio. They deliver their presentations in a group of three, and then we go over the images and ask questions on those. If the first student doesn’t know the answer, we go to the second student. So, there’s group learning during this assessment. They may not all know the same things, but it gives us a way to look at their images, give them critique/feedback, and then see where their other classmates are with some of the same objectives.
8. What are the factors to consider when selecting locations for teaching ultrasound?
Dr. Richard Hoppman: The basics of ultrasound and learning how to use the ultrasound device are best done in ultrasound laboratories with exercises and with supervision. Also, a lot of online learning material can be beneficial. So, when they get into the clinical setting, it’s very efficient and effective. I think that is in the best interest of everybody, whether it be the student, the instructor, or the patient. So we like to make sure they’re well-prepared before they get into the clinical arena.
The pandemic has caused issues for everybody, and certainly, ultrasound being a contact examination, we’ve had to change many things. We have a great deal of material that we are doing virtually. For example, we’re fortunate to have an ultrasound studio, so we do a live demonstration in the studio. Then we break up into small groups with discussion, review questions, and look at images. And that’s worked very well. The students love the hands-on learning, so we have done some scheduling to spread classes far apart where students come, and they scan themselves. Let’s say they’re going to scan the knee. They’ll wear masks, gloves, distancing, disinfect, and all those sorts of things. But I think during the pandemic, students need to get a little bit of hands-on learning to keep things going, so that’s what we’ve done.
9. What are the factors to consider when acquiring feedback while teaching ultrasound education?
Dr. Wilma Chan: We thankfully have a very rigorous and detailed way that students give feedback to us. At our medical school, we have weekly course representatives. These course reps are students who come and sit at the end of every week, and they review every lecture, every small group, and every activity in the schedule for the week. The students give very candid feedback about what they thought went well, what they thought could have gone better, and the representatives truly represent their class, so the comments filter through them.
10. How do you deal with the legal issues that may arise due to teaching ultrasound?
Dr. David Bahner: For setting up an ultrasound education program, we developed a model pool where the students would serve as models. We thought that “model” was a pejorative term, so we changed it to TSUP – Trained Simulated Ultrasound Patient.
The students would serve as models, and the paper that we wrote was TSUP – as model learner and teacher. So first, they’re a model. They learn by osmosis, by sitting there as people scan them. Then, they become teachers. Students participate voluntarily in the program; they sign a contract that says they are okay with the scanning and will speak up if anybody does any scanning that they feel uncomfortable with.
We have a safety monitor in every session, so the TSUP will sign off with the safety monitor that they are okay to model through the session. When issues come up, such as incidental findings, we have a handbook in our simulation center with a policy that talks about incidental findings where the student is responsible for working with the faculty that’s present to save that image. They then take that to their primary care physician and try to get further answers if there is any concern.
The first step is we save the images. The second is talking with the faculty that’s present, and the third is putting the onus on the student as the patient to try to contact their primary care physician and follow up. I think it’s essential when you think of some of the legal aspects and to really do your ultrasound in a way that people understand what is going on in the simulation setting. In the clinical setting, the findings go into the chart. If it happens to be an educational scan where the images are not going into the chart, and there’s an incidental finding, we will follow up with the direct team that’s taking care of that patient and inform them so they can get the appropriate testing or have the patient follow up.
Participants:
Dr. Richard Hoppmann – Clinical Professor of Internal Medicine, Director of the Ultrasound Institute/Dean Emeritus, Ultrasound Institute, School of Medicine Columbia
Dr. David Bahner – Professor of Emergency Medicine, Ultrasound Division Chief, Department of Emergency Medicine, The Ohio State University
Dr. Wilma Chan – Assistant Professor of Clinical Emergency Medicine, Department of Emergency Medicine, Perelman School of Medicine, University of Pennsylvania