AI-Assisted LVEF vs. Cardiac MRI
2025 Validation Study in Italy
A recent prospective study in the Journal of Clinical Medicine offers compelling evidence that portable, artificial intelligence-assisted ultrasound can now match the precision of Cardiac Magnetic Resonance (CMR) imaging. While CMR is widely regarded as the gold standard for quantifying left ventricular ejection fraction (LVEF) due to its superior resolution and lack of geometric assumptions, access to it remains limited. This research sought to determine if a compact, AI-driven device could provide a reliable bedside alternative.
Table of Contents
The “Gold Standard” Test
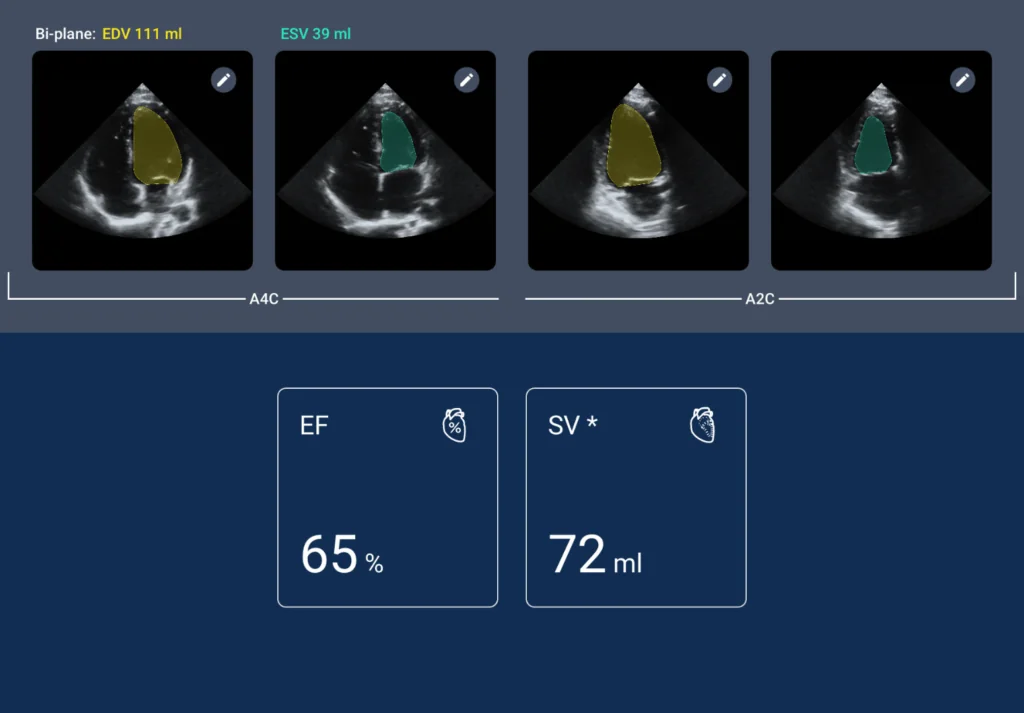
The study enrolled 49 adult patients scheduled for clinically indicated CMR at a single center in Italy. Participants underwent both the standard MRI scan and a bedside echocardiogram using the Kosmos device. This portable tool utilizes deep learning algorithms to automatically identify end-systolic and end-diastolic frames, calculating LVEF in approximately five seconds without requiring a gated electrocardiogram. To ensure rigorous comparison, nearly three-quarters of the patients underwent both imaging procedures on the same day.
Performance and Reliability
The findings revealed a remarkable level of agreement between the portable AI assessment and the advanced MRI imaging. The median LVEF derived from the AI-assisted ultrasound was 55 percent, compared to 57 percent for the CMR, a difference that was not statistically significant.
Linear regression analysis demonstrated a Pearson correlation coefficient of 0.99, indicating an exceptionally strong relationship between the two modalities. Furthermore, Bland-Altman analysis showed a mean bias of just 1.1 percent. These metrics suggest that the AI algorithm is highly accurate and does not systematically overestimate or underestimate heart function compared to the reference standard.
Critical Nuances and Limitations
While the data supports the reliability of the device, the researchers noted specific limitations. Discrepancies between the AI and MRI methods were slightly more pronounced at higher ejection fraction values. The authors suggest this may be due to the difficulty of delineating endocardial contours in a vigorously contracting heart where papillary muscles and trabeculae are prominent.
The study also emphasized that the AI algorithm produces a raw numerical value without interpreting the clinical context. It cannot account for critical variables such as severe valvular disease, arrhythmia, or hemodynamic instability. Additionally, the system’s accuracy remains heavily dependent on image quality. Performance may suffer in patients with poor acoustic windows, such as those with obesity or chronic lung disease, who were largely excluded from this initial validation to ensure optimal comparison conditions.
Critical Nuances and Limitations
This validation suggests that AI-powered point-of-care ultrasound may be poised to democratize high-level cardiac diagnostics. By delivering results comparable to MRI in seconds, these tools could revolutionize triage in emergency departments and intensive care units where time is a critical factor. The ability to obtain gold-standard-level data at the bedside may significantly reduce the need for more time-consuming and expensive standard echocardiography in routine screening scenarios.
References
- Bisignani G, Volpe L, Madeo A, Vico R, Bencardino D, De Bonis S. AI-Assisted LVEF Assessment Using a Handheld Ultrasound Device: A Single-Center Comparative Study Against Cardiac Magnetic Resonance Imaging. Journal of Clinical Medicine. 2025; 14(13):4708. https://doi.org/10.3390/jcm14134708
Q&A: LVEF vs MRI
The study found an exceptionally high level of accuracy, with a Pearson correlation coefficient of 0.99 between the two methods. The difference in results was not statistically significant, showing a mean bias of only 1.1%, suggesting that the portable AI device can match the precision of the “gold standard” MRI in quantifying heart function.
The primary benefits are speed and accessibility. While a Cardiac MRI is expensive and often requires a scheduled appointment, the AI-driven device (like the Kosmos used in the study) can provide results at the bedside in approximately five seconds. It does not require a gated electrocardiogram, making it an ideal tool for rapid triage in emergency rooms or intensive care units.
Yes. The AI’s performance is highly dependent on the quality of the ultrasound image. It may struggle with patients who have “poor acoustic windows,” such as those with obesity or chronic lung disease. Additionally, the study noted that the AI can be slightly less precise at very high ejection fractions, where a vigorously contracting heart makes it harder for the algorithm to trace the internal borders of the heart.
No. The researchers emphasized that the AI provides a raw numerical value (the LVEF percentage) but cannot interpret the clinical context. It does not account for complex factors like severe valvular disease, arrhythmias, or hemodynamic instability. It is designed to be a tool that assists healthcare providers, not a replacement for comprehensive clinical evaluation.