FAST Exam:
How a POCUS Protocol Changed Trauma Care
In the trauma bay, where every second matters, clinicians once relied on physical examinations, time consuming scans, and invasive procedures to diagnose internal injuries, leading to delays in diagnosis and management, clinical errors, and higher mortality and morbidity.
The introduction of the Focused Assessment with Sonography for Trauma (FAST) exam marked a significant change in emergency medicine. By using ultrasound at the bedside, clinicians gained the ability to quickly and non-invasively assess patients for internal bleeding. Today, the FAST exam and its successor, the eFAST exam, are standard components of trauma assessment, improving patient outcomes and reducing the need for unnecessary invasive procedures.
This article covers the history of this protocol, from the technological discoveries that made it possible to its evolution into the eFAST exam used in modern trauma care.
Table of Contents
Trauma Care Before FAST: Reliance on Exam Findings
Before bedside ultrasound, the approach to trauma care was guided by two main protocols: the Primary Survey (or ABCDEs) and the Secondary Survey. The purpose of these surveys was to help physicians quickly assess a patient and determine the likelihood of severe injuries and internal bleeding.
The Primary Survey consisted of five assessments:
- Airway: Ensuring the patient’s airway is stable and open
- Breathing: Assessing respiratory effort and gas exchange to confirm the patient can breathe properly
- Circulation: Checking blood pressure and pulse for signs of shock or bleeding
- Disability: Conducting a neurological assessment to identify any deficits resulting from the trauma
- Exposure: Fully exposing the patient for examination while preventing hypothermia
If the patient was stabilized, a Secondary Survey would follow, involving a detailed trauma history and a comprehensive physical examination.While these surveys were the standard of care, they could not always detect internal bleeding with certainty. For hemodynamically unstable patients, the next step was often an invasive procedure known as diagnostic peritoneal lavage (DPL), while highly sensitive, was also associated with higher complication rates.1 DPL involved making a surgical incision into the abdomen to check for blood and frequently led to “blank laparotomies”—surgeries where no significant injury was found. This older method highlighted a need for a tool that was quick, accurate, repeatable, non-invasive, and available at the point of care.
The Technological Leap: Paving the Way for a New Protocol
The development of the FAST exam was dependent on earlier advances in ultrasound technology. The scientific principle, the piezoelectric effect, was discovered by brothers Pierre and Jacques Curie in 1880. This effect, which describes how certain materials generate an electric charge in response to mechanical stress, is the basis of ultrasound technology.
These principles were first applied to medicine in the mid-20th century, with early uses during WW2. The development of real-time ultrasound scanners in the 1970s and gray-scale imaging options in the 1980s were important steps forward. The invention of color flow Doppler ultrasound in the 1980s further expanded the technology’s capabilities, allowing clinicians to visualize blood circulation within the body. These advancements made ultrasound devices more practical for clinical use and laid the groundwork for the development of the FAST exam.
The Birth and Adoption of the FAST Exam
ED physicians started to use USG during the 1980s and a need for standardized protocols was borne. Ultimately, FAST exam was coined in 1993 it rapidly became a recognized strategy in trauma assessment.2 The Focused Assessment with Sonography for Trauma (FAST) exam was designed to address the limitations of traditional trauma evaluations. Its primary goal was the rapid identification of free fluid—usually blood—within a patient’s abdominal cavity. The initial protocol focused on three areas: the right upper quadrant (RUQ), the left upper quadrant (LUQ), and the pelvic view.The protocol offered significant advantages. It was non-invasive, could be performed quickly at the bedside, and gave trauma teams immediate insight into a patient’s condition. By 2001, the American College of Emergency Physicians (ACEP) had established comprehensive guidelines for its use, solidifying its role as a standard of care.3
The Evolution to eFAST: Expanding the View
The success of the FAST exam quickly led to its evolution.
In 2004, the exam was extended to include imaging of the chest. This addition allowed for the detection of other trauma complications like hemothorax (blood in the chest cavity) and pneumothorax (a collapsed lung). This expanded protocol became known as the Extended FAST (eFAST) exam.4
The modern eFAST exam allows a trained clinician to assess a patient for free fluid or air in the abdomen, pericardium, and chest in approximately three to five minutes. As general surgeon and POCUS proponent Dr. Josè Pinto states, a clinician can become proficient in identifying abnormalities with 20-30 exams, making it an effective and accessible tool for guiding immediate decisions.
The eFAST Exam in Modern Trauma Care
Today, the eFAST exam is a key component of trauma care. It is typically performed alongside the Primary Survey to diagnose or rule out internal bleeding at a more rapid rate during the initial screening. While CT scans remains a standard diagnostic method for trauma patients, they require time and transport. For hemodynamically unstable patients, a positive FAST exam may be the deciding factor that allows them to bypass the CT scanner and go straight to the operating room.
The exam is indicated in cases such as:
- Trauma patients who are hemodynamically unstable
- Patients who have experienced penetrating or blunt trauma to the abdomen or thorax
- Trauma patients who were previously stable but have experienced a rapid worsening of their symptoms
The advantages of using POCUS for trauma assessment are clear5. It is:
- Non-invasive: It does not involve radiation or surgical incisions.
- Quick and Dynamic: The exam provides real-time information at the bedside.
- Repeatable: It can be performed multiple times to monitor a patient’s condition.
- Cost-effective: It offers an economical imaging solution compared to other modalities.
The Future of Trauma Assessment
The shift from relying on physical signs and invasive procedures to the rapid information provided by the eFAST exam represents a significant improvement in patient care. This evolution, driven by scientific and clinical innovation, has helped reduce clinical errors and allowed many patients to avoid unnecessary invasive procedures.
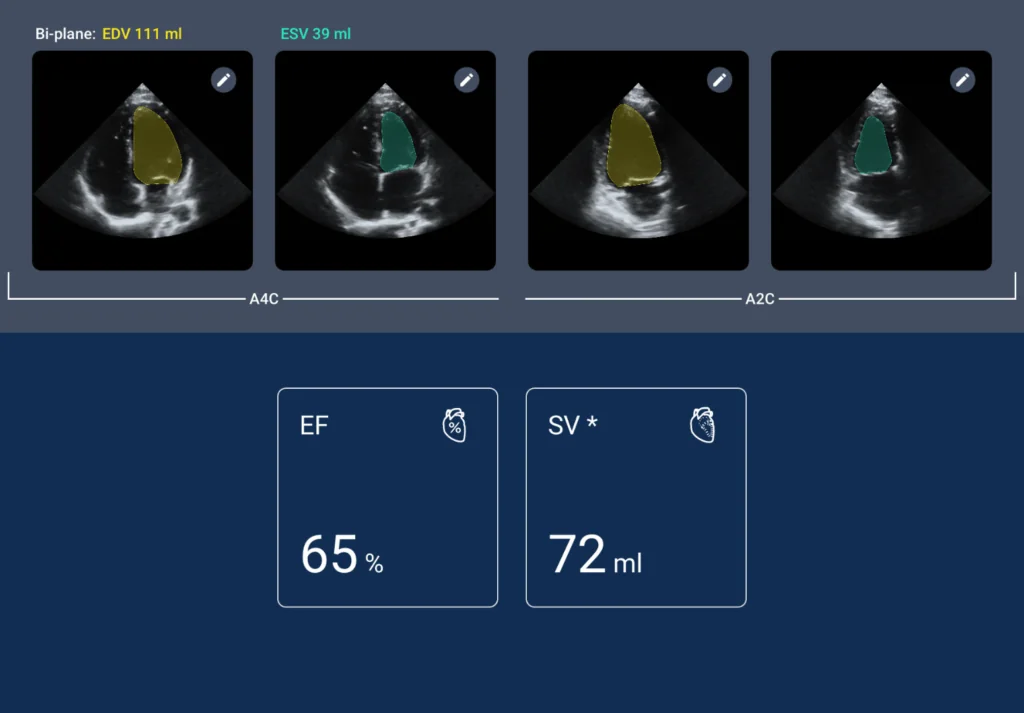
As technology advances, the role of POCUS in medicine will continue to grow and become similar to a stethoscope. The integration of artificial intelligence into ultrasound systems, such as the AI-driven features available on the Kosmos ultrasound system from EchoNous, may help flatten the learning curve and make these tools more accessible. By providing anatomical labeling and automated measurements, AI can help build confidence for new users and enhance efficiency for experienced ones. The story of the FAST exam is a testament to how technology can reshape medical practice.
The FAST exam, or Focused Assessment with Sonography for Trauma, is a rapid bedside ultrasound protocol used to quickly detect internal bleeding in trauma patients. It helps clinicians make faster, life-saving decisions.
eFAST stands for Extended Focused Assessment with Sonography for Trauma. Unlike the traditional FAST exam, eFAST includes chest imaging to identify pneumothorax and hemothorax, improving trauma assessment accuracy.
FAST and eFAST exams provide fast, non-invasive, and repeatable assessments of internal bleeding and thoracic injuries. They reduce the need for invasive procedures, lower diagnostic delays, and improve patient outcomes.
FAST identifies free fluid in the abdomen and pelvis, while eFAST adds detection of hemothorax, pneumothorax, and pericardial effusion. Some injuries may still require further imaging for confirmation.
Yes. FAST and eFAST exams are non-invasive, radiation-free, and can be repeated multiple times to monitor changes in a patient’s condition.
References
- Falcone RE, Wanamaker SR, Santanello SA, Carey LC. Safety and efficacy of diagnostic peritoneal lavage performed by supervised surgical and emergency medicine residents. Eur J Emerg Med. 1997;4(3):150-155. doi:10.1097/00063110-199709000-00007
- Tsui CL, Fung HT, Chung KL, Kam CW. Focused abdominal sonography for trauma in the emergency department for blunt abdominal trauma. Int J Emerg Med. 2008;1(3):183-187. doi:10.1007/s12245-008-0050-2
- American College of Emergency Physicians. Emergency ultrasound guidelines. Ann Emerg Med. 2009;53(4):550-570. doi:10.1016/j.annemergmed.2008.12.013
- Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST). J Trauma. 2004;57(2):288-295. doi:10.1097/01.ta.0000133565.88871.e4
- Stengel D, Rademacher G, Ekkernkamp A, Güthoff C, Mutze S. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2015;(9):CD004446. doi:10.1002/14651858.CD004446.pub4