Beyond a Good Squeeze:
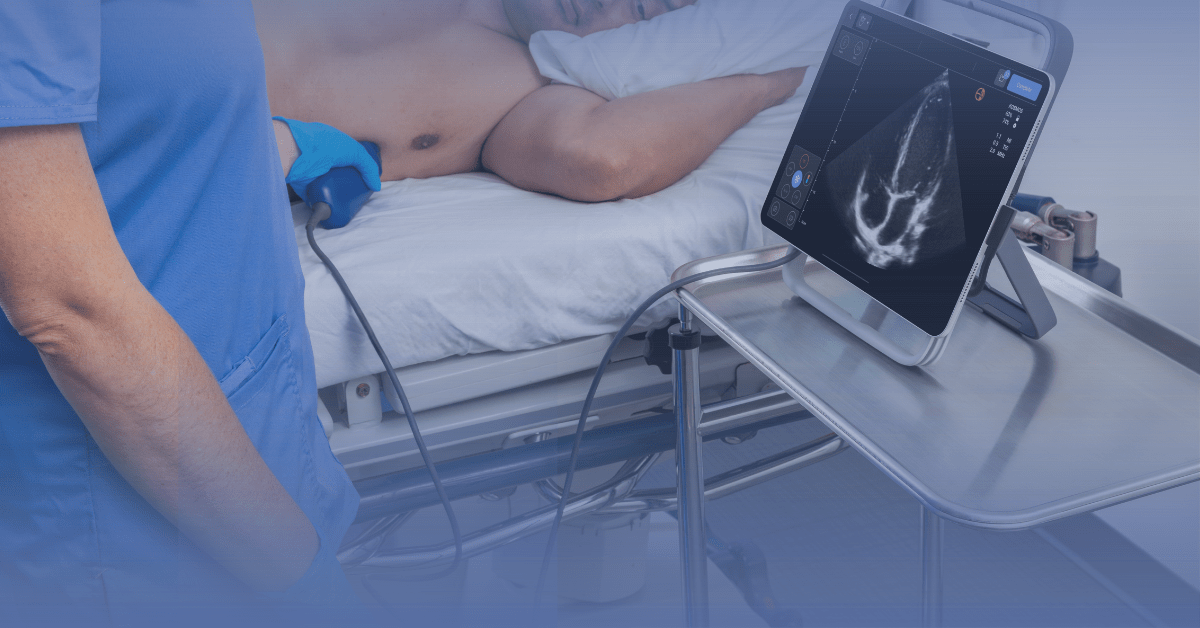
How to Get LVEF on Kosmos Three Ways
For decades, clinicians have honed the skill of “eyeballing” a cardiac ultrasound—assessing the left ventricle’s “squeeze” to estimate its function. This rapid, qualitative assessment is a testament to clinical experience, and has been shown to be relatively accurate [1]. But, in an era of precision medicine, critical decisions regarding diagnosis, management, and device-based therapies increasingly depend on a definitive number both from an evidence and sometimes payor standpoint [2].
That number is the Left Ventricular Ejection Fraction (LVEF).
LVEF is a fundamental measure of the heart’s pumping power, reflecting the percentage of blood the left ventricle ejects during systole in relation to the end-diastolic volume [1]. It is widely recognized as a critical marker of global systolic function and one of the “strongest predictors of cardiovascular outcomes” [2, 3]. The calculation is a ratio of stroke volume (the amount of blood pumped out) to the end-diastolic volume (the amount of blood in the ventricle before it pumps), expressed as a percentage [2].
Table of Contents
Why an Accurate LVEF Matters
An accurate LVEF measurement is essential for diagnosing, managing, and risk-stratifying a wide range of cardiac conditions [2]. Its most prominent role is in the assessment and classification of heart failure, which directly dictates therapeutic pathways [2]. Guidelines categorize patients based on LVEF into heart failure with reduced (HFrEF, LVEF ≤40%), mildly reduced (HFmrEF, LVEF 41-49%), or preserved (HFpEF, LVEF ≥50%) ejection fraction [2].
This quantitative classification is pivotal. LVEF is also a primary criterion for risk stratification; for example, a low LVEF is a critical threshold for considering an implantable cardioverter-defibrillator (ICD) for the primary prevention of sudden cardiac death [2,4]. Furthermore, LVEF assessment is essential after myocardial infarction, in the management of valvular heart disease, and for monitoring patients receiving cardiotoxic chemotherapy [2]. In short, it is a number that directly facilitates diagnosis and management in settings from the CCU and Emergency Department to outpatient consultations [3].
Three Quantitative LVEF Methods on Kosmos
Moving beyond the subjective “eyeball” is critical for accurate documentation, serial tracking, and therapy qualification. The Kosmos platform provides multiple quantitative pathways to obtain this vital metric.
Method 1: Auto EF Biplane Simpson’s Method (The Gold Standard)
This is the flagship, AI-driven method on Kosmos and is the 2D method recommended by the American Society of Echocardiography [2]. The Kosmos platform uses this biplane method of disks (Modified Simpson’s rule), which involves analyzing the ventricle in two separate views: the apical 4-chamber (A4C) and the apical 2-chamber (A2C) [2, 5].
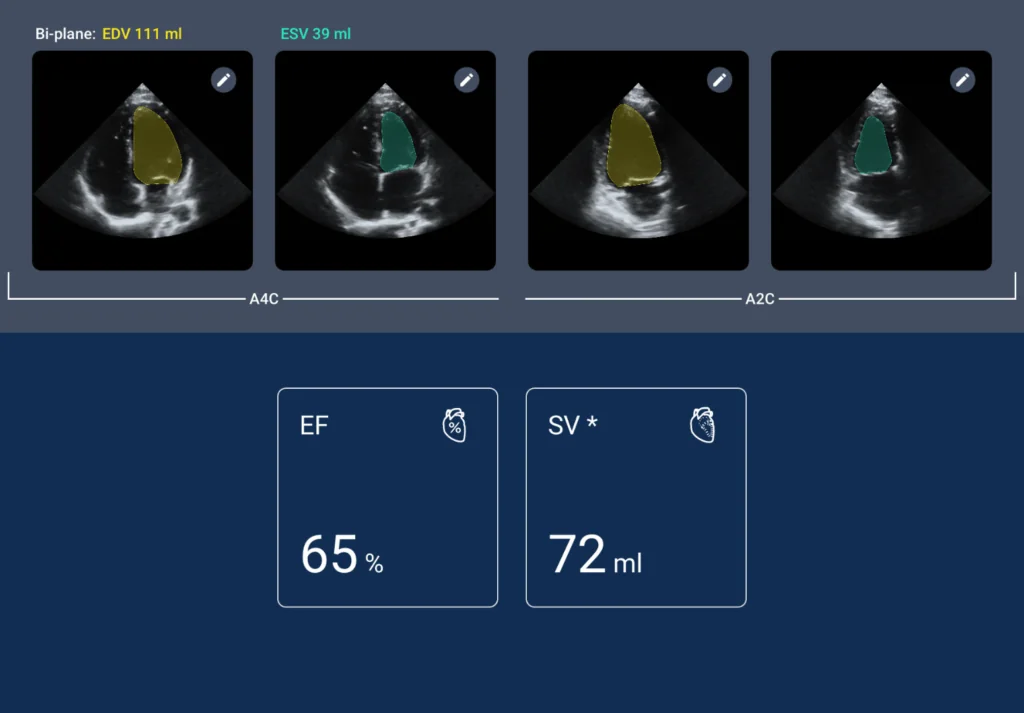
The Kosmos workflow is designed for speed and simplicity. The user acquires clips of the A4C and A2C views, and the AI algorithm automatically identifies the end-diastolic and end-systolic frames, traces the endocardial borders, and calculates the LVEF [5]. A clinical benchmarking study found this automated LVEF can be obtained in less than 20 seconds, a dramatic improvement over the 2-3 minutes often required for manual tracing on a cart-based system [3].
This method’s accuracy has been validated in real-world settings. A 2023 prospective, multicenter study published in npj Digital Medicine found that the Kosmos AI-assisted LVEF provided “highly reproducible LVEF estimations” when compared to formal transthoracic echocardiograms (TTEs), achieving an overall intraclass correlation (ICC) of 0.904 [5]. Crucially, the AI empowered novice users, who achieved an ICC of 0.921, demonstrating the platform’s ability to deliver expert-level accuracy to a wider range of clinicians [5].
Method 2: The Teicholz Method (The Classic PLAX Calc)
This is a classic echocardiographic calculation available on the Kosmos platform. The Teicholz method does not use the apical views, but instead relies on the parasternal long-axis (PLAX) view [2].
Using M-mode or 2D calipers from the PLAX view, the clinician measures the left ventricular internal diameter at its widest point in diastole (LVIDd) and its narrowest point in systole (LVIDs) [2]. The Kosmos calculation package then applies the Teicholz formula to these linear measurements to estimate the ventricular volume and ejection fraction [2].
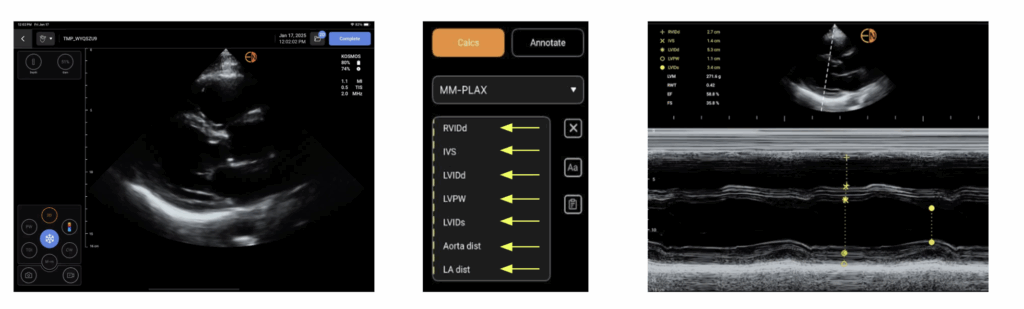
This method is fast and convenient, requiring only a single view. However, it is important to know its limitations. The Teicholz method relies on major geometric assumptions about the heart’s shape. Therefore, it is known to be less accurate in patients with an irregularly shaped ventricle or, significantly, in those with regional wall motion abnormalities (which are common in ischemic heart disease) [2].
Method 3: AI-Assisted Single-Plane Simpson’s
For technically difficult imaging of the apical two-chamber, there is an optional choice to skip this view. In some clinical scenarios, obtaining a textbook-quality A2C view is challenging or time-consuming.
In these cases, a user can still leverage the power of the Kosmos AI by using only the apical 4-chamber (A4C) view. By acquiring just the A4C clip, the AI can still perform its automated tracing and calculation, providing a single-plane Simpson’s LVEF.
This is an invaluable tool for a rapid assessment in the ED or CCU. It provides a quantitative, AI-assisted, and reproducible number that is far superior to a subjective “eyeball” guess. Like the Teicholz method, it relies on more geometric assumptions than the full biplane method [2], but it serves as a critical bridge between a qualitative guess and a full diagnostic study.
From Subjective to Quantitative
The ability to obtain a reliable LVEF at the point of care changes clinical management. As data has shown that there’s considerable variability when determining LVEF even between echocardiographic methods such as biplane vs. visual, Kosmos provides the flexibility to choose the right method for the situation [6.] Whether it’s the highly accurate, AI-driven biplane Simpson’s method (Method 1), the classic M-mode-based Teicholz calculation (Method 2), or the rapid A4C-only “secret” (Method 3), the platform empowers clinicians of all experience levels to move beyond a subjective “squeeze” to objective, quantitative data [5].
References
- Raksamani K, Noirit A, Chaikittisilpa N. Comparison of visual estimation and quantitative measurement of left ventricular ejection fraction in untrained perioperative echocardiographers. BMC Anesthesiol. 2023;23:106. doi:10.1186/s12871-023-02070-5
- Shams P, Goyal A, Makaryus AN. Left Ventricular Ejection Fraction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Sachpekidis V, Moustakidis P, Nihoyannopoulos P. Clinical benchmarking experience with the Kosmos platform, a novel AI-based handheld ultrasound system, after scanning 1200 patients in a tertiary care environment, including 600 cardiology consults. EchoNous; 2021.
- Lane C, Dorian P, Ghosh N, Radina M, O’Donnell S, Thorpe K, et al. Limitations in the current screening practice of assessing left ventricular ejection fraction for a primary prophylactic implantable defibrillator in southern Ontario. Can J Cardiol. 2010;26(3):e118-e124. doi:10.1016/S0828-282X(10)70358-5
- Motazedian P, Marbach JA, Prosperi-Porta G, et al. Diagnostic accuracy of point-of-care ultrasound with artificial intelligence-assisted assessment of left ventricular ejection fraction. npj Digit Med. 2023;6:201.
- Bayram E, Gulcu O, Aksu U, et al. Evaluating the Association Between the Three Different Ejection Fraction Measurement Techniques and Left Ventricle Global Strain. Eurasian J Med. 2018;50(3):173–177.