Dr. Adrian Wong
Intensive Care Medicine and Anesthesia
Dr. Adrian Wong and the Future of Point-of-Care Ultrasound:
An Expert’s Perspective on Improving Patient Care Through Portability, AI, and a Holistic Approach to Medicine
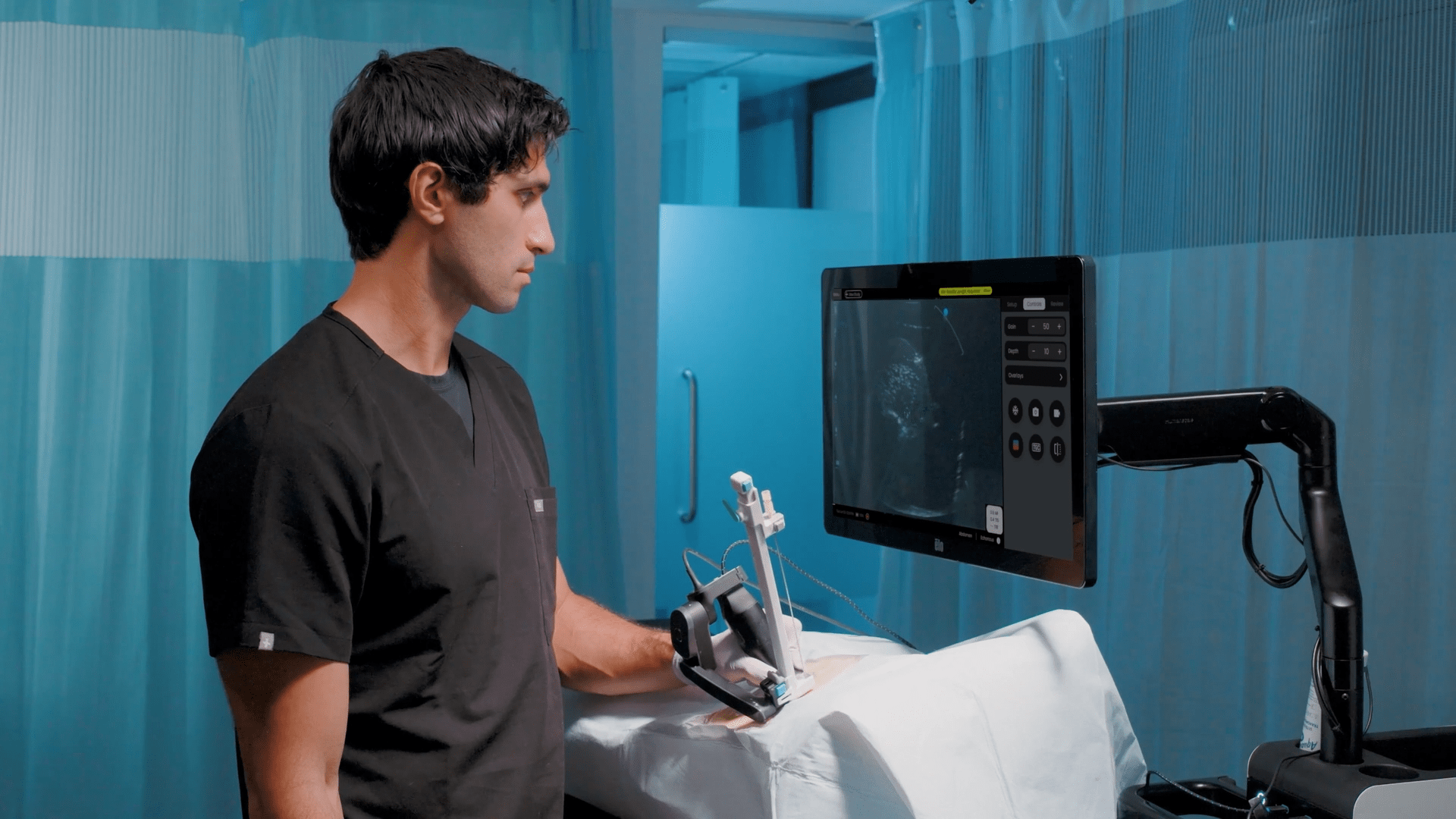
In this insightful interview, Dr. Adrian Wong, a consultant in Critical Care Medicine and Anesthesiology, provides a compelling overview of the growing role of Point-of-Care ultrasound and artificial intelligence in improving patient care. He explains how portable ultrasound devices like AI-enabled Kosmos POCUS allows clinicians to easily visualize multiple organ systems at the bedside. Dr. Wong highlights key benefits like enhanced patient engagement, more efficient training through AI-enabled real-time feedback, and the ability to combine ultrasound findings into an integrated diagnosis. Overall, he makes the case that Point-of-Care ultrasound augmented by AI will soon become an essential skill for all acute care providers seeking to optimize treatment by taking a more holistic approach to assessing their patients
Watch the video here, or read a lightly edited transcript of the interview below. Republished with the permission of Dr. Adrian Wong. This interview is edited for clarity and readability online.
Dr. Adrian Wong and the Future of Point-of-Care Ultrasound: An Expert’s Perspective on Improving Patient Care Through Portability, AI, and a Holistic Approach to Medicine
My name is Doctor Adrian Wong. I’m a consultant in Critical Care Medicine and Anesthesiologist at Kings College Hospital in London. I run our Point-of-Care ultrasound training program for all my colleagues within the department. In intensive care medicine, and indeed all acute medical specialties, POCUS becomes part and parcel of what we do. So if you look after an acutely unwell patient, there is a growing expectation, indeed a growing need, to be competent to some level in Point-of-Care ultrasound.
The reason why I think it’s very useful and helpful to the clinician is that with ultrasound it is not just a single organ system that we’re talking about. With ultrasound, we have the ability to scan the heart, we scan the lungs, we scan the abdomen, we scan the blood vessels and we put all this information together to help us better diagnose our patients and their pathology. It helps better guide our management strategies, guide our therapeutic options, such as putting in intravenous lines, because all of these organ systems work together, so you can’t really separate out the heart without thinking about its effect on the lungs, so on and so forth.
If we think about the traditional ultrasound machine, ones that tends to live in radiology departments, they’re big, they’re bulky, they stay, generally speaking, in one place. As ultrasound devices become smaller, more handheld, you can take the device and do the scans by the patient. So you go to the patients. Rather than the patient going to the radiology department and because it’s miniaturized, you increase the accessibility of the scans to the patients, but also the training opportunities for colleagues who want to learn how to scan because you can move the device and pass the device from one individual to the next much more freely, much more readily.
If you’re ill in the hospital, that already raises anxiety levels amongst patients and the beauty of Point-of-Care scanning is that when I’m performing a scan, if my patient is awake, we can show the patient the scan and talk together with them, so they have a better understanding of what we, as the medical team are looking at, what we’re trying to fix. So that I think builds better engagement and connection between the patients and the medical teams. If we take it from a training perspective, devices, such as the EchoNous Kosmos device, have lots of feedback mechanism software built into it, so that if you’re the operator, the scanner and you’re learning, the software gives you tips and tricks in terms of how you can improve the image quality image acquisition.
But traditionally I think most people think of artificial intelligence, machine learning and ultrasound in terms of making the diagnosis, and that’s again a strong feature of the Kosmos EchoNous device. This is a scan, and the software gives you more information about the scan that perhaps traditionally might not be accessible to you as the operator.
The traditional model of learning a scan is that you as an individual will have to find a mentor, you go and build up a log book of cases, of scans, pathologies, so on and so forth and you go away, find your mentor again, find your supervisor again and together you sit down, go through the scans, and if both of you have time, you might have the opportunity to scan together where your mentor is, your supervisor will tweak and change your practice. Move one rib space down, one rib space down, turn the probe this way, turn the probe that way.
But, in such a busy environment, not all of us have got the time to sit and meet together with our trainees, mentors, supervisors and so if you’ve got software that’s readily accessible with you all the time because it’s built into the machine.
The feedback is immediate, so you don’t have to go away and reflect or get a mentor to critique your scan. The software can provide feedback to you in realtime. Everything that we do with ultrasound, we want to improve patient care, patient outcome and I think, artificial intelligence, machine learning, so on and so forth, it’s just part of the equation in how we achieved that which touched upon the efficiency.
We hope the efficiency of teaching when it comes with AI, we’ve touched upon the increased information that you can get from artificial intelligence machine learning and we hope that the combination of the two ultimately leads to improved patient care.
I think the sharing of the information is a very interesting one because ultimately I do think that we will progress that way, but there’s lots of rules and regulations around cloud-based storage, especially when it comes to patient identifiers. The benefit of sharing information, collaborating between healthcare professional teams is such a strong one that I suspect that we will be working to enable sharing of information rather than restricting the sharing of information. Image records are shared between healthcare professionals in a timely, efficient manner. Certainly from a learning perspective.
As an individual training in ultrasound, trying to gain the skills set to become good at it, it’s definitely helpful because it means that the trainer and a trainee don’t have to be in the same room attached to the same device together. You’re no longer restricted by geographical distances.
Things I like about the Kosmos EchoNous device is the fact that it is portable, and the 2D image quality is very good. But I think what sets it apart, certainly from a lot of other devices available, is the fact that you’ve got Color Doppler analysis as well, and that’s particularly relevant in critical care because one of the core aspects of our job is to optimize the circulation, optimize organ perfusion and optimize heart function, and I think it’s very difficult to do that without Doppler Color analysis of the heart and blood vessels. I think that’s probably the one thing that sets it apart compared to other devices.
I believe that anyone who looks after a sick patient, looks after anyone who comes into hospital as an emergency should be able to perform some level of POCUS so the time will come where every acute physician will be able to do it. And I think the other aspect in terms of the direction of travel is that we no longer work in silos. We no longer work in a single organ system, so we don’t have people who just scan the heart, who just scan the lungs, who just scan the blood circulation. It is about bringing all this information together, because often it is attached to one single patient, one organ system dysfunction will ultimately upset the other organ systems as well, so I think the future of POCUS is inevitably that everyone will be able to learn how to scan to a certain extent. And I think we’ll be approaching it from a more holistic approach rather than individual organ systems. And ultimately, I also feel that the growing impact of artificial intelligence machine learning from a software perspective will help the clinician by treating patients better.