Resources
News & Blog
-

FAST Exam: How a POCUS Protocol Changed Trauma Care
FAST Exam: How a POCUS Protocol Changed Trauma Care In the trauma bay, where every second matters, clinicians once relied on physical examinations, time consuming scans, and invasive procedures to diagnose internal injuries, leading to…
-
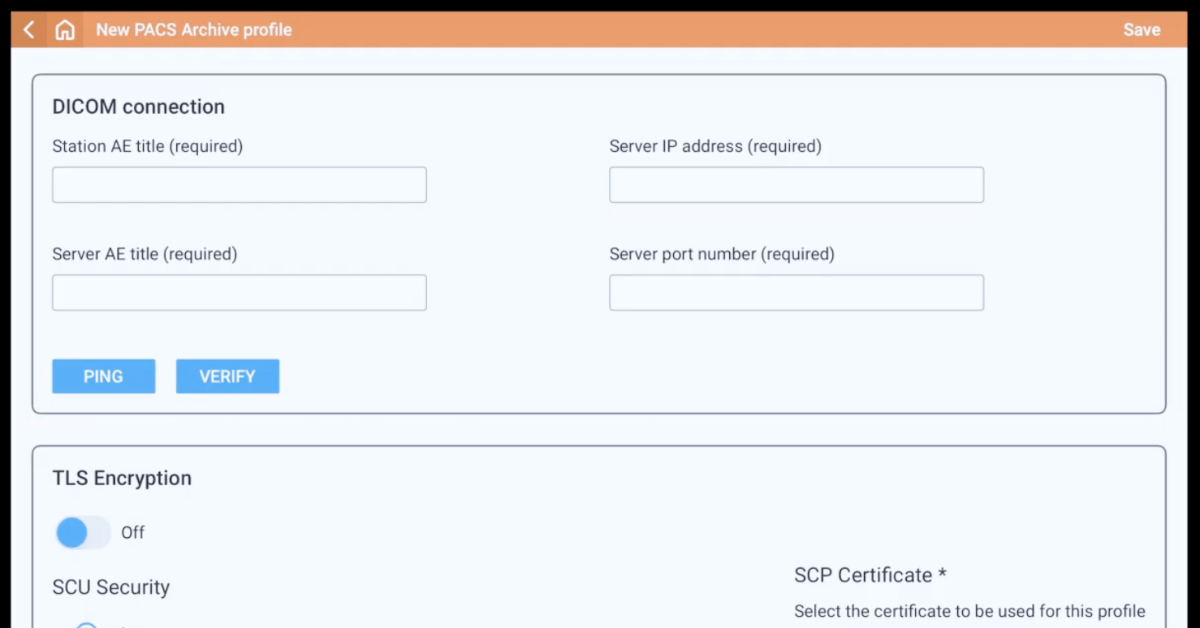
Understanding Hospital IT Infrastructure and Kosmos Ultrasound Device Integration
Understanding Hospital IT Infrastructure and Kosmos Ultrasound Device Integration Making Sense of EHRs, EMRs, DICOM, PACS, TLS, and more. The EchoNous Team For the clinician at the bedside, the primary focus is the patient. You…
-

Small Bone Fractures POCUS
POCUS First for Small Bone Fractures: A Modern, Evidence-Based Approach for Reducing X-Ray Delays and Radiation In the emergency department (ED) or acute care setting, few things are as routine as a suspected fracture of…
-

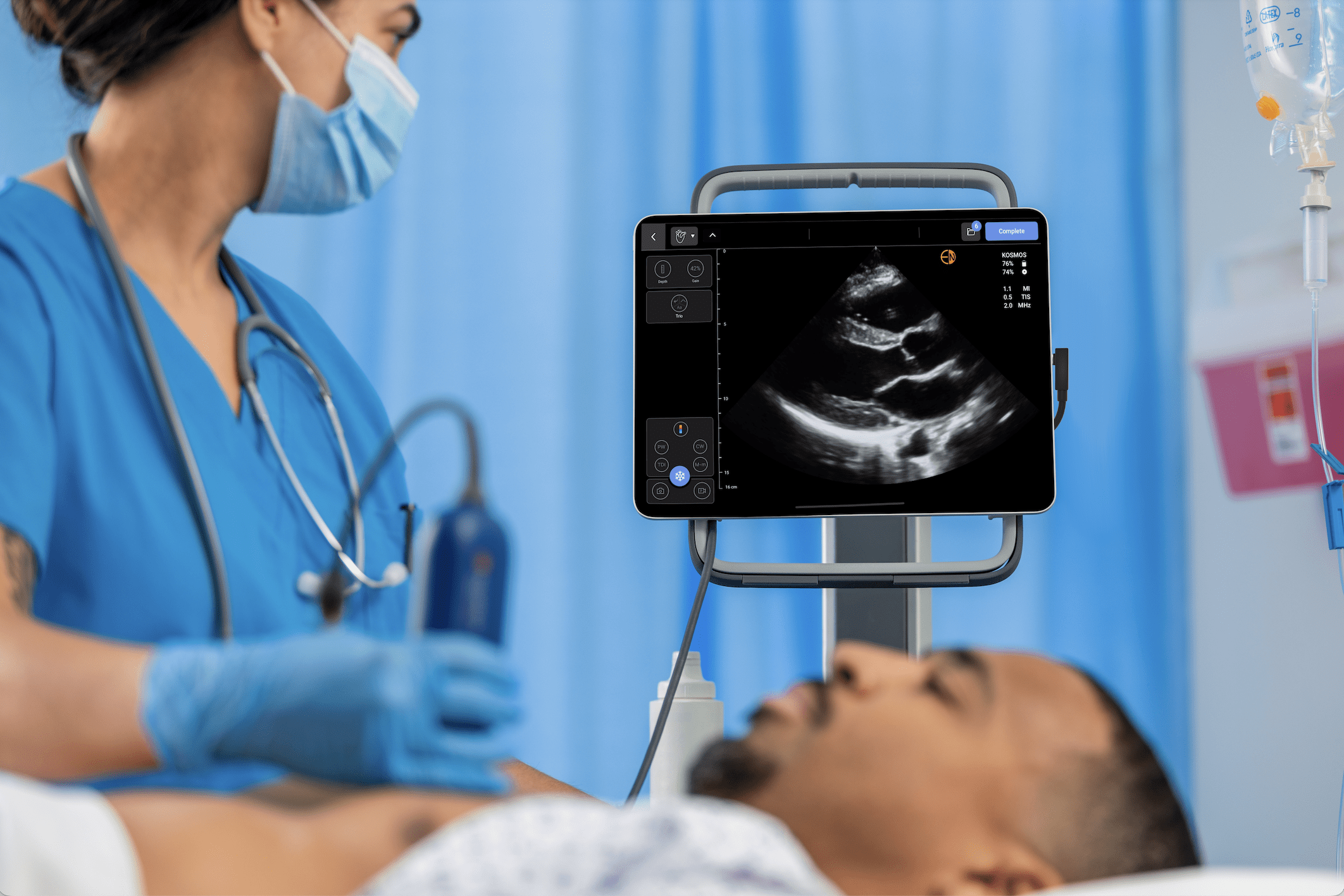
Redefining POCUS Value: Getting Cart-Level Performance Without the Cart-Level Price
Redefining POCUS Value: Getting Cart-Level Performance Without the Cart-Level Price When clinicians and administrators evaluate new point-of-care ultrasound (POCUS) devices, “best value” is a critical, multi-faceted metric. It’s not just about “what’s the cheapest probe?”…
-

From Palpation to Visualization: Why POCUS is Redefining the Lumbar Puncture
From Palpation to Visualization: Why POCUS is Redefining the Lumbar Puncture For many clinicians, the lumbar puncture (LP) is a core procedure learned by feel. Training traditionally focuses on palpating for the iliac crests, finding…
-
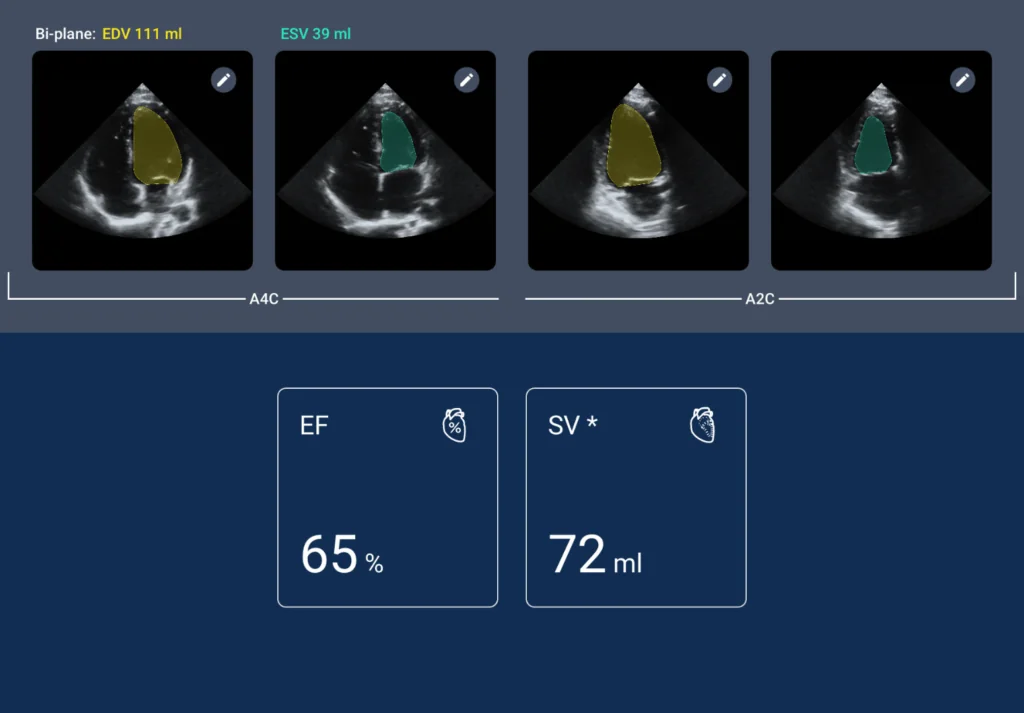
Beyond a “Good Squeeze”: How to Get LVEF on Kosmos Three Ways
Beyond a Good Squeeze: How to Get LVEF on Kosmos Three Ways For decades, clinicians have honed the skill of “eyeballing” a cardiac ultrasound—assessing the left ventricle’s “squeeze” to estimate its function. This rapid, qualitative…
-

Retropharyngeal Abscess: The Evolving Role of Bedside Ultrasound
Retropharyngeal Abscess: The Evolving Role of Bedside Ultrasound The diagnosis of a retropharyngeal abscess (RPA) represents a serious challenge in emergency medicine and pediatrics. Primarily affecting children five and younger, retropharyngeal abscess is uncommon but…
-

Turn Your POCUS Purchase into a Major 2025 Tax Deduction
Turn Your Ultrasound Investment into a Major Tax Deduction in 2025 Leveraging Section 179 and Bonus Depreciation to Lower Your Tax Bill* For many private practice owners, the cost of advanced equipment like point-of-care ultrasound…
-

Peritonsillar Abscess: The Clinical Utility of Ultrasound
Peritonsillar Abscess: The Clinical Utility of Ultrasound For any clinician, the patient with a suspected peritonsillar abscess (PTA) presents a relatively common but critical diagnostic challenge. The classic presentation of fever, severe odynophagia, trismus, and…
-
How Much Does a Point-of-Care Ultrasound Device Cost?
How Much Does a Point-of-Care Ultrasound (POCUS) Device Cost? The EchoNous Team | September 2025 Long gone are the days of point-of-care ultrasound (POCUS) being thought of as a niche tool; it’s truly become a…
-

EchoNous Appoints Tony Titus as CEO
EchoNous Appoints Tony Titus as CEO We’re thrilled to announce the appointment of Tony Titus as our new Chief Executive Officer (CEO). Tony has over 20 years of senior executive experience, bringing a proven track…
-
How to Choose a Bladder Scanner: A 4-Point Checklist for Clinical Leaders
How to Choose a Bladder Scanner: A 4-Point Checklist for Clinical Leaders In our previous guide, we explored the technology behind modern bladder scanners, their use cases in preventing unnecessary catheterizations, and the role of…
