POCUS in Family Medicine Residency Training
Point-of-care ultrasound (POCUS) has become essential for family medicine physicians, fundamentally changing how they diagnose and treat patients. Recently, it has transitioned from an optional tool to a residency training detail requirement(1). This change highlights the critical role of POCUS in improving patient care through real-time imaging and diagnostics.
Whether diagnosing cardiac issues, guiding procedures, or assessing chronic disease, POCUS equips physicians and clinicians with the skills to deliver efficient, high-quality care. This article explores the key benefits of learning ultrasound, highlights findings from recent research, and concludes with actionable steps for integrating POCUS into your practice.
Key Takeaways:
- POCUS Enhances Care: It improves diagnostic accuracy, patient outcomes, and procedural safety for family medicine physicians.
- Essential Residency Skill: POCUS experience is now a “detail requirement” in ACGME-accredited family medicine residency programs, reflecting its critical role in modern healthcare.
- Challenges and Solutions: Despite barriers like faculty training and equipment costs, integrating POCUS is achievable with the right tools and training.
Table of contents
What Is POCUS, and Why Is It Crucial?
POCUS is a portable diagnostic tool that provides immediate imaging results at the point of care. Unlike traditional imaging methods, it eliminates delays and costs associated with laboratory diagnostics or referrals(2).
In family medicine, POCUS has become a game-changer. Its versatility allows physicians to quickly assess various conditions, guide interventions, and monitor treatment effectiveness, all while improving patient outcomes(3,4)
Core Benefits of POCUS in Family Medicine
1. Accurate Diagnosis at the Point of Care
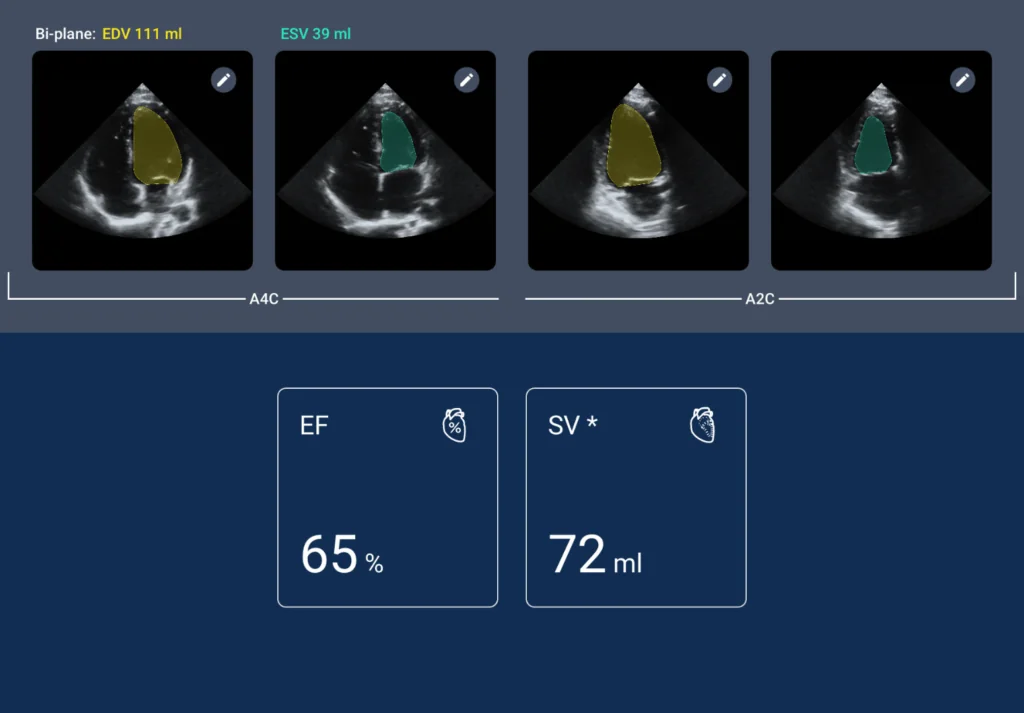
POCUS enables physicians to diagnose conditions such as pneumonia, cardiac dysfunction, and musculoskeletal injuries with unmatched precision(5). For example, ultrasound can confirm lung fluid, aiding in the quick differentiation between pneumonia and heart failure conditions that might otherwise require extensive diagnostics.
2. Enhanced Procedural Safety
Procedures such as joint aspirations, abscess drainage, and central line insertions become safer and more effective with POCUS guidance(6,7). This not only reduces complications but also increases physician confidence and patient trust.
3. Time-Saving and Cost-Effective Care
By reducing referrals and avoiding unnecessary imaging studies, POCUS streamlines care delivery. This leads to faster diagnoses and significant cost savings for patients, particularly in rural or underserved areas with limited advanced imaging(2,8).
4. Versatility Across Settings
POCUS is portable and adaptable, making it an invaluable tool in various clinical environments. Whether in urban clinics, emergency rooms, or rural settings, POCUS meets the needs of diverse family medicine practices(2,8).
Bring POCUS into your practice: Are you ready to modernize your practice? Schedule a consultation with EchoNous today to explore our cutting-edge ultrasound solutions, perfect for family medicine.
The Growing Demand for POCUS in Family Medicine Training
The importance of POCUS is reflected in its inclusion as a requirement in family medicine residency programs. Research, such as the study by Hall et al. (Family Medicine)(9), underscores its transformative impact on training and practice:
Improved Competence and Confidence:
EchoNous’ POCUS technology can significantly reduce the time required for IV insertions. The Kosmos system’s intuitive design and real-time imaging capabilities enable quick, accurate assessments of vascular structures, allowing nurses to make immediate decisions and perform insertions with confidence.
This rapid workflow enhancement translates into time savings that can be reallocated to patient care, charting, or other critical tasks, ultimately reducing the cognitive load on nurses.
Broader Scope of Practice:
Physicians trained in ultrasound can handle a wider variety of cases independently, reducing reliance on specialists and ensuring continuity of care(12,13).
Standardized Curriculum Needs:
While POCUS is increasingly integrated into residency programs, challenges such as curriculum development, faculty training, and access to equipment persist.
Read the study: Point-of-Care Ultrasound in Family Medicine Residencies 5-Year Update: A CERA Study to learn more(9).
Transforming Patient Care with POCUS
A New Era in Diagnostics
Family physicians are often the first point of contact for patients with undiagnosed conditions. POCUS enables quick, accurate evaluations that lead to immediate, effective treatments.
For example:
- A patient presenting with chest pain or shortness of breath could have a range of conditions, from pneumonia to heart failure. POCUS allows physicians to differentiate between these quickly and initiate appropriate treatment(14).
- Musculoskeletal complaints, such as joint pain or suspected fractures, are easily assessed with ultrasound, which can sometimes eliminate the need for referral to advanced imaging centers.
Chronic Disease Management Made Easier
POCUS is invaluable for monitoring chronic conditions like heart failure and liver disease. Physicians can track disease progression, adjust medications, and detect complications – all during a routine office visit. This enables proactive, patient-centered care.
Building Stronger Relationships with Patients
Real-time imaging creates an opportunity to engage patients more deeply in their care. Patients who see their condition on screen better understand their diagnosis and treatment options. This interactive approach fosters trust and encourages adherence to treatment plans.
Overcoming Implementation Challenges
Implementing POCUS in family medicine practices and training programs can be challenging despite its clear advantages. Here’s how to address these issues:
1. Curriculum Development
Residency programs must create standardized curricula that balance theoretical knowledge with practical training. This ensures new physicians graduate with the confidence and competence to use POCUS effectively(15).
2. Faculty Training
A significant barrier to implementing POCUS in residency is the need for more trained faculty. Professional development opportunities like workshops and certification programs are critical for overcoming this challenge (16).
3. Access to Technology
High-quality ultrasound devices are essential for successful POCUS integration. EchoNous provides user-friendly, innovative solutions tailored to the needs of family medicine practitioners.
The Future of Family Medicine With POCUS
Integrating POCUS into family medicine residency programs is part of a broader trend toward precision medicine. As technology advances, POCUS applications will expand, further solidifying its role in providing high-quality, patient-centered care.
For practicing physicians: A commitment to Innovation
Adopting ultrasound is more than just learning a new skill- it’s a commitment to staying at the forefront of healthcare innovation. Integrating POCUS into your practice can enhance your diagnostic capabilities, improve patient outcomes, and strengthen your practice.
Get Started With Kosmos Today
POCUS is revolutionizing family medicine. Whether you are an educator, resident, or practicing physician, now is the time to embrace this transformative technology. Schedule a consultation with EchoNous to explore how we can help you integrate Kosmos POCUS solutions into your practice or training program.
References
- Accreditation Council for Graduate Medical Education. (2023). ACGME Program Requirements for Graduate Medical Education in Family Medicine (Interim Revision effective July 1, 2024). ACGME.
- Fraleigh, C. D., et al. (2022). Point-of-care ultrasound: An emerging clinical tool to enhance physical assessment. The Nurse Practitioner, 47(8), 14.
- Do, S. (2024, April 1). Enhancing the Foundation: Dr. Steelman’s Direct Primary Care Model with POCUS. EchoNous.
- Carrera, K. G., et al. (2022). The Benefits and Barriers of Using Point-of-Care Ultrasound in Primary Healthcare in the United States. Cureus, 14(8), e28373.
- Piccioni, A., et al. (2022). Use of POCUS in Chest Pain and Dyspnea in Emergency Department: What Role Could It Have? Diagnostics, 12(7), Article 7.
- Varsha Madhavanarayanan Totadri, R. V. (2024, January 7). A Comparative Study of Drainage of Breast Abscesses by Conventional Incision and Drainage vs Ultrasound-Guided Needle Aspiration/Re-Aspiration in A Tertiary Health Care Centre. Eur J Breast Health,20(3), 194-198.
- Authors, Tran, K., et al. (2023). Point-of-Care Ultrasound for Guided Central Venous Catheter Insertion: CADTH Health Technology Review. Canadian Agency for Drugs and Technologies in Health.
- Chelikam, N., et al. (2023). Past and Present of Point-of-Care Ultrasound (PoCUS): A Narrative Review. Cureus, 15(12), e50155.
- Hall, J. W. W., et al. (2020). Point-of-Care Ultrasound in Family Medicine Residencies 5-Year Update: A CERA Study. Family Medicine, 52(7), 505–511.
- Shi, D., et al. (2019). Evaluation of a new goal-directed training curriculum for point-of-care ultrasound in the emergency department: Impact on physician self-confidence and ultrasound skills. European Journal of Trauma and Emergency Surgery, 47(2), 435.
- Hannula, O., et al. (2023). Self-reported skills and self-confidence in point-of-care ultrasound: A cross-sectional nationwide survey amongst Finnish emergency physicians. BMC Emergency Medicine, 23(1), 23.
- Andersen, C. A., et al. (2019). Point-of-Care Ultrasound in General Practice: A Systematic Review. Annals of Family Medicine, 17(1), 61.
- Onsongo, L. N., et al. (2025). Perspectives of health care providers on obstetric point-of-care ultrasound in lower-level health facilities in Kenya. Midwifery, 140, 104196.
- Martinez, E. C., et al. (2023). Point-of-Care Ultrasound for the Diagnosis of Frequent Cardiovascular Diseases: A Review. Cureus, 15(12), e51032.
- Brown, C. M., et al. (2021). An Integrated Multispecialty Curriculum for Point-of-Care Ultrasound. Advances in Clinical Medical Research and Healthcare Delivery. 1(3).
- Nathanson, R., et al. (2022). Development of a Point-of-Care Ultrasound Track for Internal Medicine Residents. Journal of General Internal Medicine, 37(9), 2308.