The Economic Benefits of Integrating Ultrasound in Community Hospitals
In October 2021, NHS England issued a Press Release establishing 40 diagnostic centers across England. Financing for these centers is backed by a P350 million investment, with a plan to provide about 2.8 million scans in the first year of operation (1). Commenting on the implementation strategy for this plan, the UK Department of Health and Social Care wrote:
“… these centers will help to achieve earlier diagnoses for patients through easier, faster, and more direct access to the full range of diagnostic tests needed to understand patients’ symptoms”
Although this move directly improved equitable access to diagnostic services, it is only one of many. For instance, the implementation of the Medicare Modernization Act in 2003 by the United States government negatively affected chemotherapy infusion revenues; it however triggered investments in innovative imaging technologies like positron emission tomography and ultrasound (2).
Both instances critically emphasized the need for medical imaging modalities with diverse applications in community hospitals. Today, many countries have care access initiatives promoting AI-assisted chest X-rays for tuberculosis and point-of-care ultrasound (POCUS) services for emergency specialists, intensivist, and cardiologists. Despite these programs, a gap exists in the diagnostics capabilities of level 3 and 4 rural hospitals globally.
In November 2020, eClinicalMedicine published a report investigating the capacity of diagnostic services including radiology and pathology in hospitals providing high-quality surgical, anesthetic, and obstetric care in Mexico and Brazil. The stratified cross-sectional study found that facilities in low-resource, rural communities often lack functional diagnostic services (3). Another survey from 10 countries also estimated that only 1.2% of rural primary care hospitals had ultrasound capabilities (4).
Key Takeaways:
- Although the global healthcare outlook has improved in recent years, a huge gap still exists in the diagnostic landscape; rural community hospitals especially still lack modern imaging capabilities.
- Ultrasound systems present huge economic benefits to these hospitals including improved diagnosis accuracy rates, reduced length of hospital stays, increased patient satisfaction, and expedited therapy.
- Rural community hospitals face a huge barrier in acquiring, installing, and maintaining conventional cart-based ultrasound systems; they are expensive and bulky to store.
- Kosmos, an EchoNous offering in modern, ultraportable ultrasound, presents a perfect fit and cheaper alternative to cart-based ultrasound systems for rural community hospitals.
Table of contents
Why Integrate Ultrasound Capabilities in Community Hospitals?
Without adequate imaging and diagnostics services, patient management largely relies on empiric treatment and syndromic inferences. WHO guidelines recommend routine chest X-rays and Ultrasound sessions as diagnostic gold standards for diseases of public health priority and organ-system malfunctions. For instance, multiple scientific evidence supports ultrasound in the diagnosis of pneumonia, a disease common in underserved, low-income communities.
Beyond merely complying with diagnosis guidelines, ultrasound capabilities benefit patient care and professional development in rural community hospitals. These benefits may include:
1. Improved Diagnosis Accuracy Rates
Ultrasound modalities serve diagnostics purposes in almost every branch of modern medicine. In fact, the WHO disease-specific guidelines published between 2012 and 2023 established ultrasound as the gold-standard diagnostic option in at least a dozen conditions including cardiovascular health, maternal care, and neonatal health.
Recently, AI-enabled labeling and contract capabilities have significantly expanded the range of ultrasound usage in public health. Today, ultrasound modalities have significantly improved the diagnostic accuracy rate of hepatic diseases (5), acute dyspnea (6), breast cancer (7), and other diseases of public health priority. In community hospitals, the adoption of bedside ultrasound modalities is projected to significantly improve clinicians’ decision-making.
2. A Cost-efficient, Versatile Imaging Option
Compared with conventional imaging modalities like X-ray, magnetic resonance imaging, and computed tomography, point-of-care ultrasound is cheaper, portable, versatile, and easily accessible. Its safety and ultrafast features make it the best imaging fit for a rural community hospital.
Leveraging recent advancements in imaging technologies, POCUS brands boast huge computing and data processing capabilities and signal-processing algorithms that have rapidly expanded their use beyond traditional radiology and cardiology practices (8). Considering the variety of conditions reported in community hospitals, POCUS presents the most cost-effective diagnostics option.
3. Expedited Treatment Course
Improved diagnosis accuracy expedites treatment course. For instance, early, accurate diagnosis in cancer therapy is linked with faster therapy initiation and an improved 5-year survival rate (9). Ultrasound imaging and labeling capabilities help clinicians decide quickly on a treatment regimen, shortening patients’ length of hospital stays and expediting treatment course.
4. Increased Patient Satisfaction Rates
In 2019, Semergen published a multi-center study analyzing patient satisfaction levels when undergoing bedside ultrasound performed by a family physician. Conducted in Madrid between December 2015 and March 2016, this study evaluated how patients interacted with different POCUS modalities. The study showed that the level of ‘satisfied-very satisfied” reached 95% (10).
Patients opt for POCUS based on its portability, speed, and image-enhancement capabilities. Many other studies also show how increased satisfaction rates positively influenced patient outcomes.
5. Reduction in Readmission Rate
Readmission and the economic cost of disease burden are two closely linked metrics. A high trend of re-admission directly projects an increased cost of healthcare services in the near future. In rural community hospitals, readmission rates across specialties are a big deal; they impact resource allocation, funding, and institutional reputation.
POCUS streamlines diagnosis sessions for many patients on appointment, helping clinicians make informed, accurate decisions on disease severity and the need for outpatient care plans. As a versatile and fast imaging option, POCUS can help rural community hospitals efficiently control readmission rates.
Financing an Ultrasound System
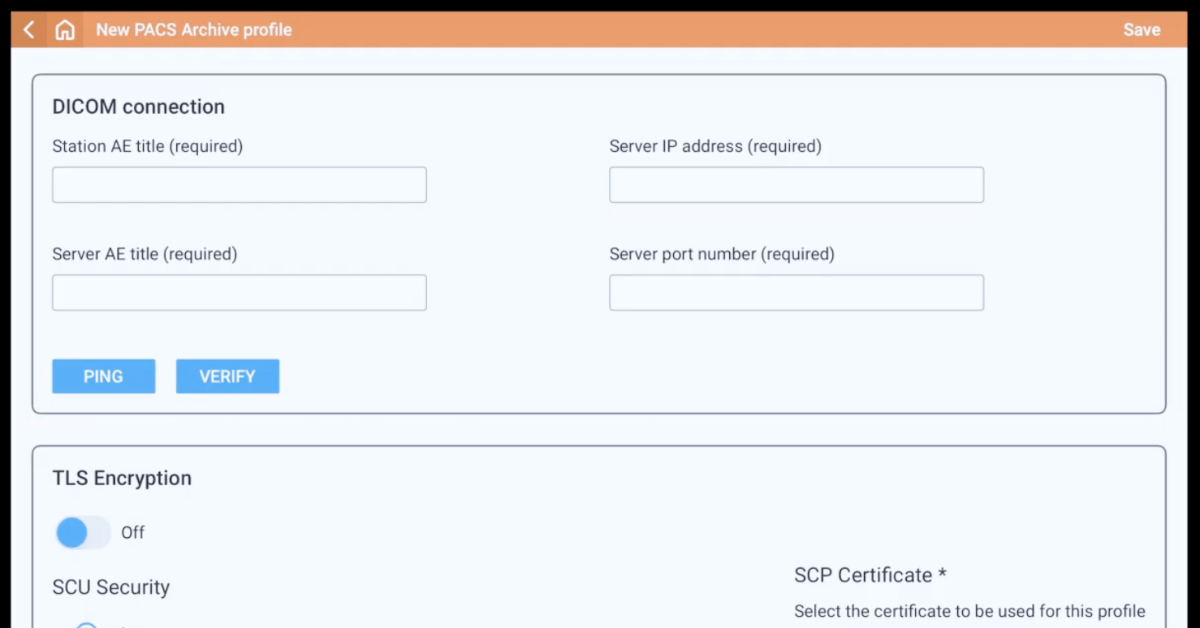
Setting up a hospital-wide imaging system requires huge capital investment. The invested capital is expected to cover more than just purchase costs; the cost of training, installation, maintenance, and operational kits is included. Hospital administrators are expected to conduct an internal study of orders, payers mix, and insurance coverage of the patient population.
Metrics like these accurately picture investment size, funding options, and ultrasound needs. Compact ultrasound systems may cost as high as $73, 797 (11). With personnel, software maintenance, upgrades, and installation costs, investment per unit may cost up to $2 million per site. Compared with conventional compact ultrasound systems, POCUS systems are relatively cheaper.
Kosmos for Community Hospitals: Choosing an Affordable Option
Point-of-care ultrasound systems present huge economic benefits for rural community hospitals. With the rapid adoption of POCUS modalities globally, low-cost, versatile options serve these hospitals more efficiently.
The Kosmos System represents a best-in-class option, with its versatility, portability, and advanced imaging features. Schedule a Kosmos demo today to get started with a perfect imaging option for community hospitals that is cheaper than typical cart-based ultrasound systems.
References
- Department of Health and Social Care, NHS England, and The Rt Hon Sajid Javid MP. 40 community diagnostic centers launching across England. 2021. GOV.UK. https://www.gov.uk/government/news/40-community-diagnostic-centres-launching-across-england (accessed 25 Dec 2024).
- Diagnostic imaging in community practice. (2006). Journal of Oncology Practice, 2(3), 113–115. https://doi.org/10.1200/JOP.2006.2.3.113
- Roa, L., Moeller, E., Fowler, Z., Vaz Ferreira, R., Mohar, S., Uribe-Leitz, T., Guilloux, A. G. A., Mohar, A., Riviello, R., Meara, J. G., Souza, J. E. D. S., & Macias, V. (2020). Assessment of diagnostics capacity in hospitals providing surgical care in two Latin American states. EClinicalMedicine, 29-30, 100620. https://doi.org/10.1016/j.eclinm.2020.100620
- Yadav, H., Shah, D., Sayed, S., Horton, S., & Schroeder, L. F. (2021). Availability of essential diagnostics in ten low-income and middle-income countries: results from national health facility surveys. The Lancet. Global health, 9(11), e1553–e1560. https://doi.org/10.1016/S2214-109X(21)00442-3
- Nam, K., Torkzaban, M., Halegoua-DeMarzio, D., Wessner, C. E., & Lyshchik, A. (2023). Improving diagnostic accuracy of ultrasound texture features in detecting and quantifying hepatic steatosis using various beamforming sound speeds. Physics in medicine and biology, 68(4), 10.1088/1361-6560/acb635. https://doi.org/10.1088/1361-6560/acb635
- Papanagnou, D., Secko, M., Gullett, J., Stone, M., & Zehtabchi, S. (2017). Clinician-Performed Bedside Ultrasound in Improving Diagnostic Accuracy in Patients Presenting to the ED with Acute Dyspnea. The western journal of emergency medicine, 18(3), 382–389. https://doi.org/10.5811/westjem.2017.1.31223
- Su, S., Ye, J., Ke, H., Zhong, H., Lyu, G., & Xu, Z. (2024). Multimodal ultrasound imaging: a method to improve the accuracy of sentinel lymph node diagnosis in breast cancer. Frontiers in oncology, 14, 1366876. https://doi.org/10.3389/fonc.2024.1366876
- Wang, S., Hossack, J. A., & Klibanov, A. L. (2020). From Anatomy to Functional and Molecular Biomarker Imaging and Therapy: Ultrasound Is Safe, Ultrafast, Portable, and Inexpensive. Investigative radiology, 55(9), 559–572. https://doi.org/10.1097/RLI.0000000000000675
- Crosby, D., Bhatia, S., Brindle, K. M., Coussens, L. M., Dive, C., Emberton, M., Esener, S., Fitzgerald, R. C., Gambhir, S. S., Kuhn, P., Rebbeck, T. R., & Balasubramanian, S. (2022). Early detection of cancer. Science (New York, N.Y.), 375(6586), eaay9040. https://doi.org/10.1126/science.aay9040
- Pertierra-Galindo, N., Salvo-Donangelo, L., Salcedo-Joven, M. I., Román-Crespo, B., & Froilán Torres, M. C. (2019). Estudio de satisfacción del paciente ante la realización de una ecografía en atención primaria [Study of patient satisfaction when performing an ultrasound in Primary Care]. Semergen, 45(4), 239–250. https://doi.org/10.1016/j.semerg.2018.08.007
- America Hospital Association. (May, 2024). America’s Hospitals and Health Systems Continue to Face Escalating Operational Costs and Economic Pressures as They Care for Patients and Communities. https://www.aha.org/costsofcaring