Transforming Cardiology with Point-of-Care Ultrasound:
A Conversation with Dr. Peter Fitzgerald

Dr. Peter Fitzgerald
MD, PhD

Luke Baldwin
VP of Global Marketing, EchoNous
Luke Baldwin, VP of Global Marketing at EchoNous, had the privilege of sitting down with Dr. Peter Fitzgerald, MD, PhD, a renowned interventional cardiologist and a leader in healthcare technology. In this informative conversation, we dig into the fascinating intersection of artificial intelligence (AI) and point-of-care ultrasound (POCUS), exploring the transformative potential of these technologies within the constantly evolving healthcare arena.
[Note: This interview has been edited for clarity and brevity.]
Introduction
Dr. Fitzgerald’s journey demonstrates the significant promise of point-of-care ultrasound (POCUS) and artificial intelligence in healthcare. Combining his expertise as a physician and engineer, he offers a unique perspective on the evolution of ultrasound technology and its implications for assessing heart health.
Journey and Background
Luke Baldwin: Before we dive in, Peter, I’d like to set the stage. Could you please introduce yourself, tell us about your background, and give us a sense of your experience?
Peter Fitzgerald, MD: My journey into the world of healthcare and ultrasound began with a computer science PhD and a stint at Hewlett-Packard. During my time there, I had the opportunity to work on early ultrasound technology, including massive machines like the 7702A. This experience ignited my passion for ultrasound’s potential, particularly in the context of heart assessment.
My journey took an unexpected turn when Hewlett-Packard sponsored my medical school education in Boston. Balancing medical school and my ongoing association with ultrasound technology, particularly with the Andover group, gave me a unique perspective. I was involved in developing software and graphics card components, solidifying my roots in this field.
After medical school, I specialized as an interventional cardiologist at UCSF and spent over two decades on the faculty at Stanford. Throughout my career, ultrasound remained a constant companion. We even delved into intravascular ultrasound, which allowed us to see blood vessels from the inside out, a novel perspective compared to traditional transthoracic echocardiograms.
This journey led us into the heart, where we visualized percutaneous procedures like aortic valve replacements and mitral valve repairs. To perform these procedures successfully, it’s crucial to have clear visibility, similar to headlights on a car.
What excites me most, though, is the transformation happening in medical education. Medical students are transitioning from stethoscopes to point-of-care ultrasound (POCUS), marking a significant shift. I like to draw an analogy between this transition and the shift from Blockbuster to Netflix. POCUS is no longer limited to doctors and nurses; it’s becoming accessible to everyone. It empowers individuals to conveniently monitor their heart health, whether they have concerns or already diagnosed cardiac conditions. This evolution is truly remarkable in the healthcare landscape.
Evolution of Ultrasound in Cardiology
Luke Baldwin: You have a unique way of explaining this, probably better than anyone I’ve spoken to. I’ve been involved in the point-of-care ultrasound field for about 15 years now, but your perspective, as both an engineer who worked on early ultrasound systems and a physician who has used and benefited from them in diagnosing patients with heart conditions, is truly insightful. I’m curious if, at a high level, you could take us through the evolution over time. We started with large cart-based systems that few people knew how to operate, and then came the introduction of POCUS machines just over 20 years ago. More recently, we’ve transitioned to handheld devices, and now AI is entering the picture. Could you walk us through the history of ultrasound in cardiology?
Peter Fitzgerald, MD: When I reflect on it, it’s a bit quirky, to be honest. Hewlett and Packard sponsored my journey through medical school, and two decades later, I found myself caring for them in the Coronary Care Unit at Stanford. It felt like a meaningful, full-circle moment.
Echo rooms posed a challenge for me as I often found myself dozing off due to the dark and quiet environment. As our cardiac procedures became more intensive, we relied on echo techs for assistance, but scheduling coordination remained challenging. I always felt there had to be a better way. As we started performing more intensive cardiac procedures, we would call in echo techs for assistance, especially with intraoperative echocardiography (ICE). Yet, the logistical disconnect remained. For instance, we’d need an echo tech to assess a patient’s effusion in the ICU, and there was always the challenge of coordinating schedules.
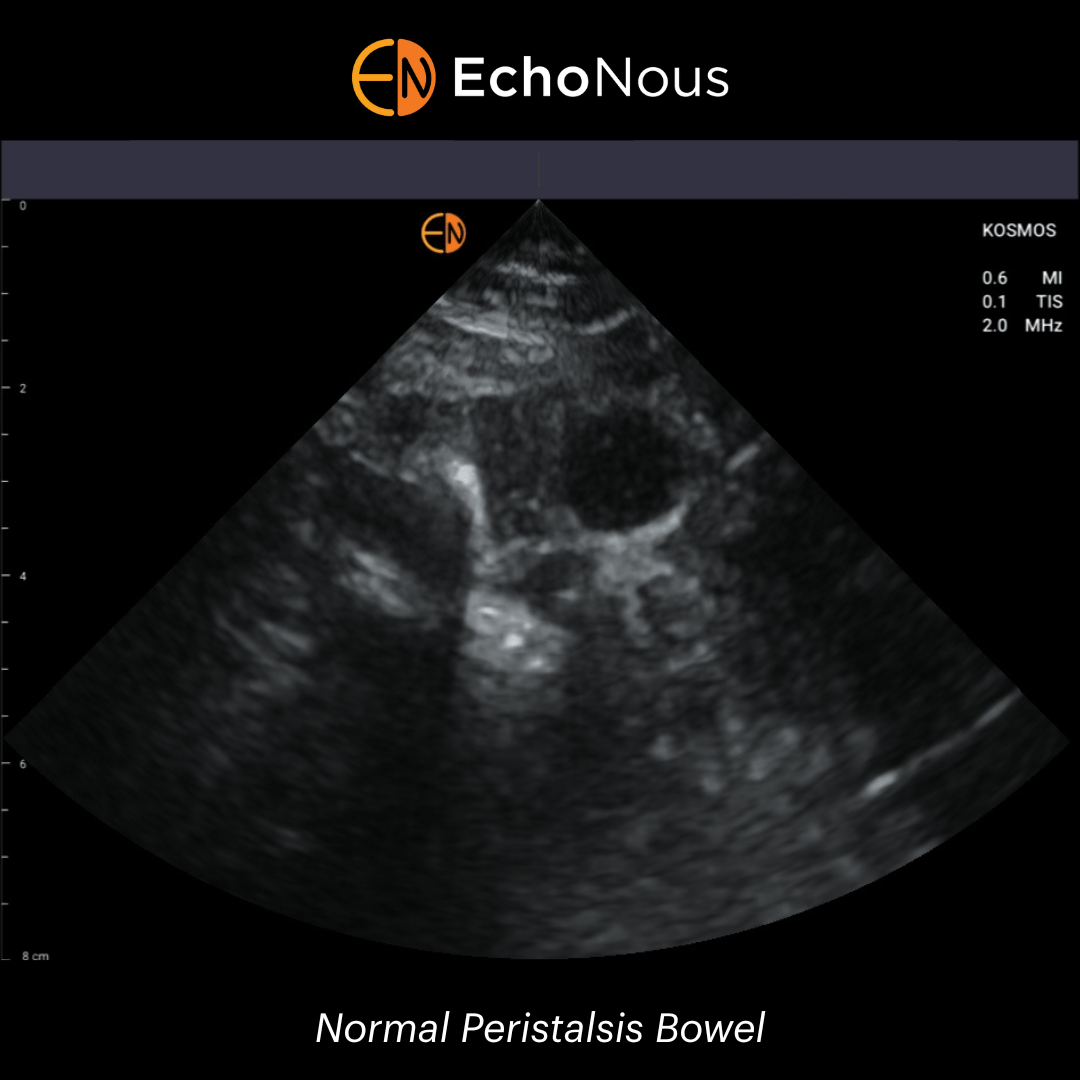
Imaging technology has advanced significantly, making things more seamless within hospitals. Today, residents can pull up a chest X-ray on their cell phones. Imaging rounds have evolved, and the convenience of mobile access has transformed how we approach these matters. With POCUS becoming handheld and highly accessible, it holds the potential to truly transform healthcare. What excites me the most is the prospect of conducting heart-healthy scans remotely. This could bridge the gap of understanding for many people and lead to more efficient and timely referrals within the healthcare system.
Currently, the process involves multiple steps—starting with a family practitioner, then a primary care provider, followed by a cardiologist who might suggest an echo. It’s like asking a car mechanic if you need a new muffler. These steps can cause anxiety and are not always efficient. I’m enthusiastic about simplifying these pathways, especially since referral mechanisms in healthcare systems have seen some changes during the pandemic. As they adapt and potentially become more streamlined, we can navigate these transitions more effectively.
Patient Pathways and Reducing Anxiety
Luke Baldwin: You’ve highlighted a couple of key points here. Once patients enter that healthcare pathway, there’s a series of steps. They visit their family physician, receive a referral, consult with a cardiologist, undergo an ultrasound examination, consult with the cardiologist again, and finally, speak with their physician about the next steps. The time it takes from the initial visit to defining a treatment plan could be weeks and that doesn’t account for the time that the patient dealt with their issue before deciding to get seen in the first place. Can this timeline be compressed?
Peter Fitzgerald, MD: You bet. We experience the benefits and convenience of advanced technology in most other areas of life, so why not in healthcare? More people actually die from cardiovascular disease than cancer. So, when I see patients with cardiovascular concerns, I understand that time is of the essence and anxiety is a real factor.
Today, I use tele-health with patients on their couches, but I ensure other family members are present. I show them their EKG, angiogram, and echo and point out what we’re concerned about or what has improved. This engagement is a crucial puzzle piece that POCUS brings to the table.
Empathy and the Future of Healthcare
Luke Baldwin: You mentioned Anxiety. Anxiety comes in when there’s an absence of knowledge, don’t you think? If you don’t know what’s going on, if you don’t know if it’s a problem, or if you don’t know what the answer is, that leaves a lot of room for you to come up with these dire scenarios.
Peter Fitzgerald, MD: For sure. So, when they see that echo, when they see that regurgitant jet and the family sees it, it defuses all the other things they’ve built up in their mind. I think that some of these technologies help us with that part. And, God forbid, we probably could be more empathetic and not wait until AI does it.
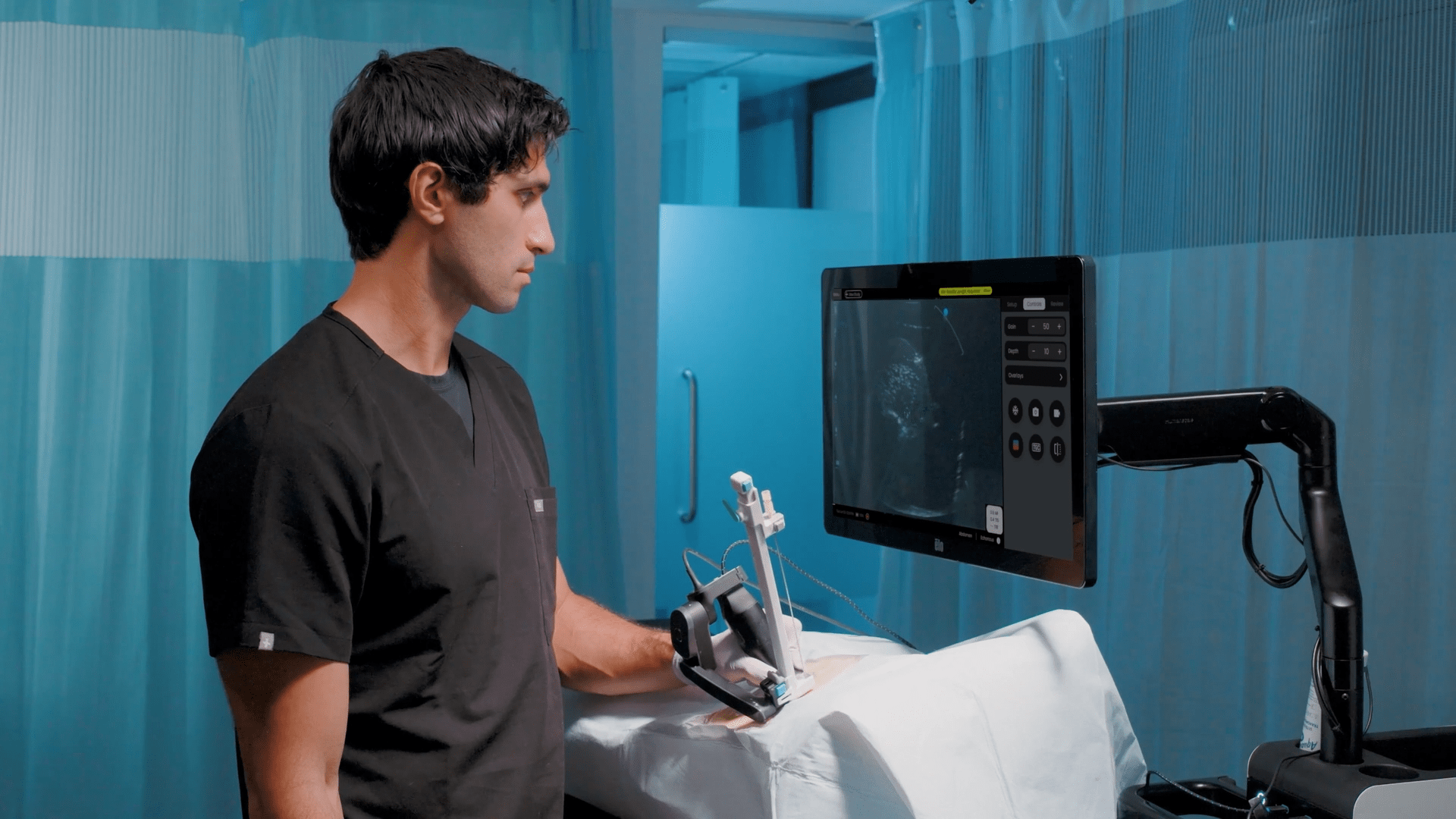
Luke Baldwin: So, I’m curious to hear your thoughts on the current process that, as you’ve outlined it, hasn’t completely changed. That timeline today that we see both pre-visit and post-visit is the reality for most people. How do you see that changing in the future, and what role do folks like us at EchoNous, with our Kosmos product, with the AI we’re developing, what role can we play to help change the reality that people experience today?
Peter Fitzgerald, MD: Absolutely, that’s precisely the point. Lowering the divide between diagnosis and therapy is essential. We aim to make them balanced and expand our screening to cover a more extensive population. Various companies have ventured into assessing cardiovascular risk through blood tests, which is admirable. However, these methods often involve imputations.
When we directly focus on the heart, there’s significant potential. Imagine if we could identify individuals on the path to heart failure earlier, possibly even before they reach a critical stage. Treating them with a heart failure drug combined with weight loss could prove highly effective. The synergistic power of addressing both aspects is undeniable, as many people aspire to lose weight to some extent.
What truly excites me is the concept of a continuum of care. In reality, continuity often falls short in healthcare. For example, if I perform five coronary cases on a Monday, I might only remember the names of two patients. Continuity of care is frequently lacking, and episodic care is prevalent. To enhance healthcare outcomes, we must involve a broader range of healthcare professionals, from physician assistants to nurses.
This is vital because the U.S. spends more on healthcare but has a shorter life expectancy. We’re losing half a year each year, and our maternal mortality rate is alarmingly high. 90 million people have hypertension that remains uncontrolled due to the lack of continuity of care. While we have drugs and episodic diagnostics, we need more continuity of care and tools to support it. Your device, among others, offers a direct heart assessment, requiring just five pieces of information for effective triage and potentially earlier diagnosis of individuals with cardiovascular issues.
Resistance may arise, but I’d consider running all new patients through a heart-healthy scan in clinical settings, this can take as little as 5 minutes. This process could become even more efficient over time. As long as there’s a payment system in place, it offers a comprehensive experience.
Challenges and Opportunities in Healthcare
Luke Baldwin: That’s remarkable. I spend more time on paperwork before my visit than the amount of time it would take to conduct the heart-healthy scan you described.
Peter Fitzgerald, MD: That’s why I’m enthusiastic about this. It’s not without challenges, though. We face reimbursement issues and need to engage with stakeholders in the payment industry who often take an actuarial approach. However, identifying problems earlier in the healthcare process may ultimately impact downstream costs. Actuarial arguments can resonate with payers and be a significant driver for adoption.
Furthermore, this technology brings in non-traditional players like Microsoft, Oracle, Walmart, and Amazon, which possess unique capabilities, particularly in their interactions with payers. These industry giants could accelerate the democratization of ultrasound in peripheral settings, and I find that prospect promising.
Luke Baldwin: Absolutely. Beyond that, consider populations struggling to access healthcare. It’s not limited to rural areas in the US but extends globally. In many countries, there’s a severe shortage of cardiologists, and these devices, combined with AI, can play a crucial role. They enable non-experts to capture images and send reports to specialists, reducing the dependence on a single region’s resources. It could have a significant impact.