Point-of-Care Ultrasound (POCUS):
Bridging Healthcare Gaps in Rural Communities

Dr. Liliana Garcia Aguilar
General Practitioner

Luke Baldwin
VP of Global Marketing, EchoNous
Luke Baldwin, VP of Global Marketing at EchoNous, recently connected with Dr. Liliana Aguilar, a general practitioner committed to improving healthcare outcomes in high-risk rural areas, specifically in Santa Maria Ozolotepec, Mexico. Join us as we explore the impact of Point-of-Care Ultrasound (POCUS) on breaking down barriers and providing timely and accurate medical care for underserved communities in rural areas.
Dr. Liliana Garcia Aguilar serves as the sole physician in the remote community of Santa Maria Ozolotepec, Mexico, where she has spent 16 years in her role as a general practitioner.
[Note: This interview has been edited for clarity and brevity.]
Bridging Healthcare Gaps in Rural Oaxaca
Luke Baldwin: Dr. Liliana, it’s great to meet you. To start, could you share a bit about yourself—your clinical training and where you work?
Liliana Aguilar, MD: Good morning, my name is Liliana Garcia Aguilar. I am a general practitioner and have worked for 16 years in the rural community of Santa Maria Ozolotepec, Mexico. It’s a pleasure to meet you, and I am very happy to share my experiences here. I’m so glad you are interested in the rural community of Oaxaca.
Luke Baldwin: Could you describe the community and patients that you serve?
Liliana Aguilar, MD: Santa Maria Ozolotepec, is a small rural community with about 1,100 people. We only have this health center. I am the only doctor, and we have two nurses.
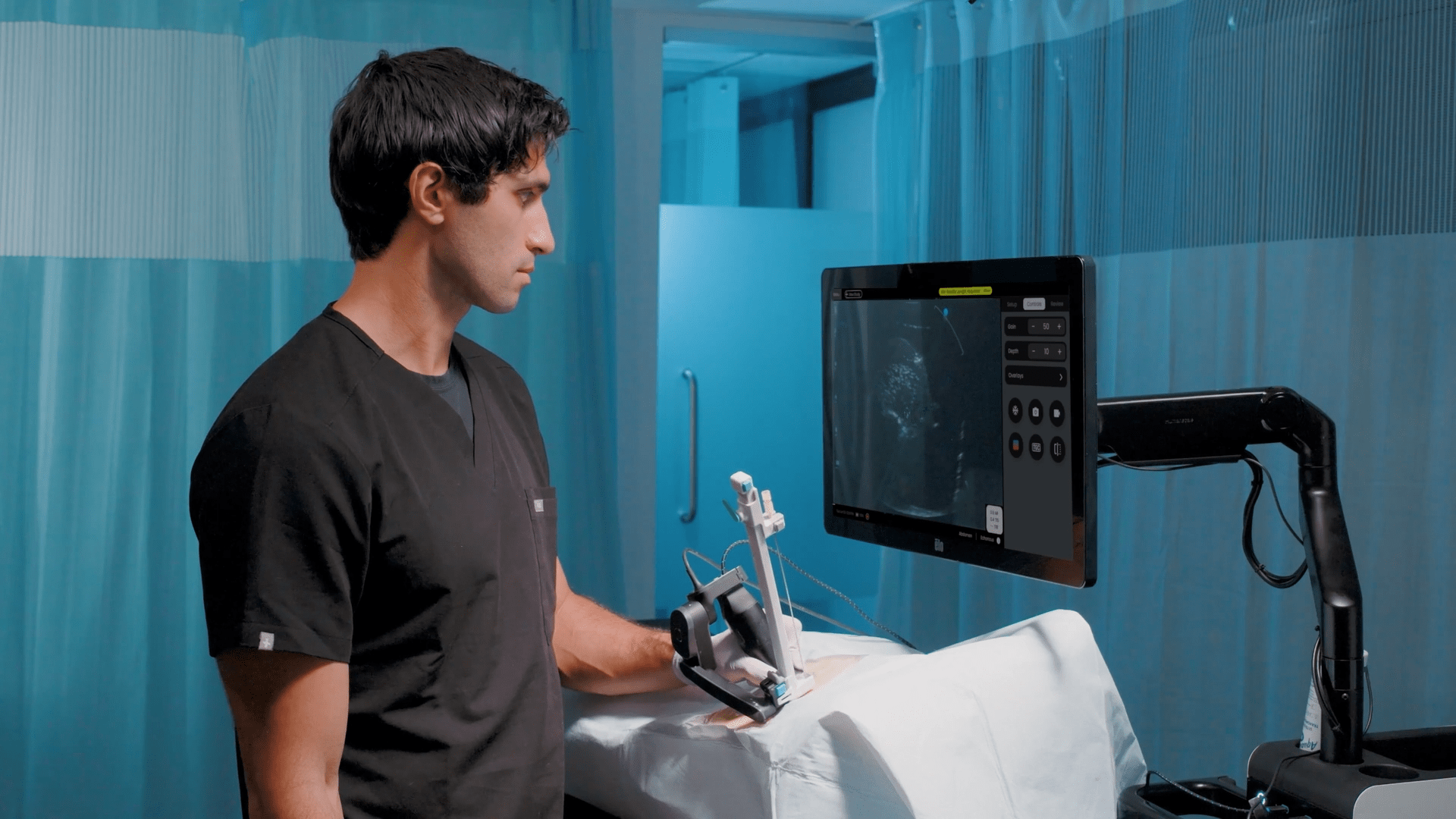
Almost two years ago, we embraced the opportunity to access satellite internet and telemedicine services from 19Labs, which utilizes EchoNous as its POCUS solution, as part of a project by the Oaxaca State Health Department. This has proven incredibly beneficial. The point-of-care ultrasound (POCUS) equipment has become an essential tool, facilitating the technological support we provide to patients in need, marking a significant technological leap for healthcare services in our remote location, which is near Guatemala.
[Because we are] situated about two hours from Miahuatlan, our nearest hospital, this internet service enables fast ultrasound connections, crucial for critical ultrasound cases.
What can I say? I could spend the whole day sharing beautiful stories about the tremendous support we’ve been able to provide. The cases that have benefited patients, saving lives – it’s truly great support.
POCUS: Addressing High-Risk Needs in Rural Healthcare
Luke Baldwin: To follow up on the high mortality risk, is it for the mother or the baby? And what are the typical causes? Is it related to breech birth or placenta previa? I’m curious about the specific reasons behind it.
Liliana Aguilar, MD: Sometimes, it’s the mother’s life at greater risk and other times, it’s the baby’s, depending on the mother’s diagnosis. We frequently deal with preeclampsia and its severe form, eclampsia, as well as obstetric hemorrhage with uterine atony, posing serious threats to mothers.
It’s important to talk with patients about warning signs that could indicate potential complications and stress the importance of timely medical attention. With the help of technology, we can connect patients with gynecologist consultations through telemedicine. Recently, there was a case where timely transfer for preeclampsia was made possible through telemedicine. Ultrasounds also play a critical role in identifying placental problems early.
In the past 16 years, only two maternal deaths occurred, but none since 2011. Financial constraints and limited access to ultrasounds pose challenges, but telemedicine helps bridge these gaps, ensuring prompt care and diagnoses. The absence of deaths isn’t without challenges—pathologies like uterine atony hemorrhages, preeclampsia, and eclampsia occurred but were detected and managed in time. The new technology aids quick ultrasounds, facilitating immediate action and transfers with gynecologist guidance via tablets.
Our goal is to keep patients stable and save lives, even those reluctant to leave. With the support from specialists, significant strides have been made in achieving these outcomes.
Luke Baldwin: Do consultations involve ultrasound exams for preeclampsia? How does ultrasound help, and what pathologies can be identified in time?
Liliana Aguilar, MD: With ultrasound, we can identify preeclampsia early, as early as week 20, by observing calcification in the placenta. We can also assess amniotic fluid levels, detect issues like oligohydramnios or polyhydramnios, and determine the baby’s position. For example, if it’s headfirst, breech, transverse, or feet-first. Ultrasound helps us assess risks for maternal death, such as the baby not coming headfirst, which can complicate delivery.
Luke Baldwin: You have a certificate in ultrasound. How does that support your work?
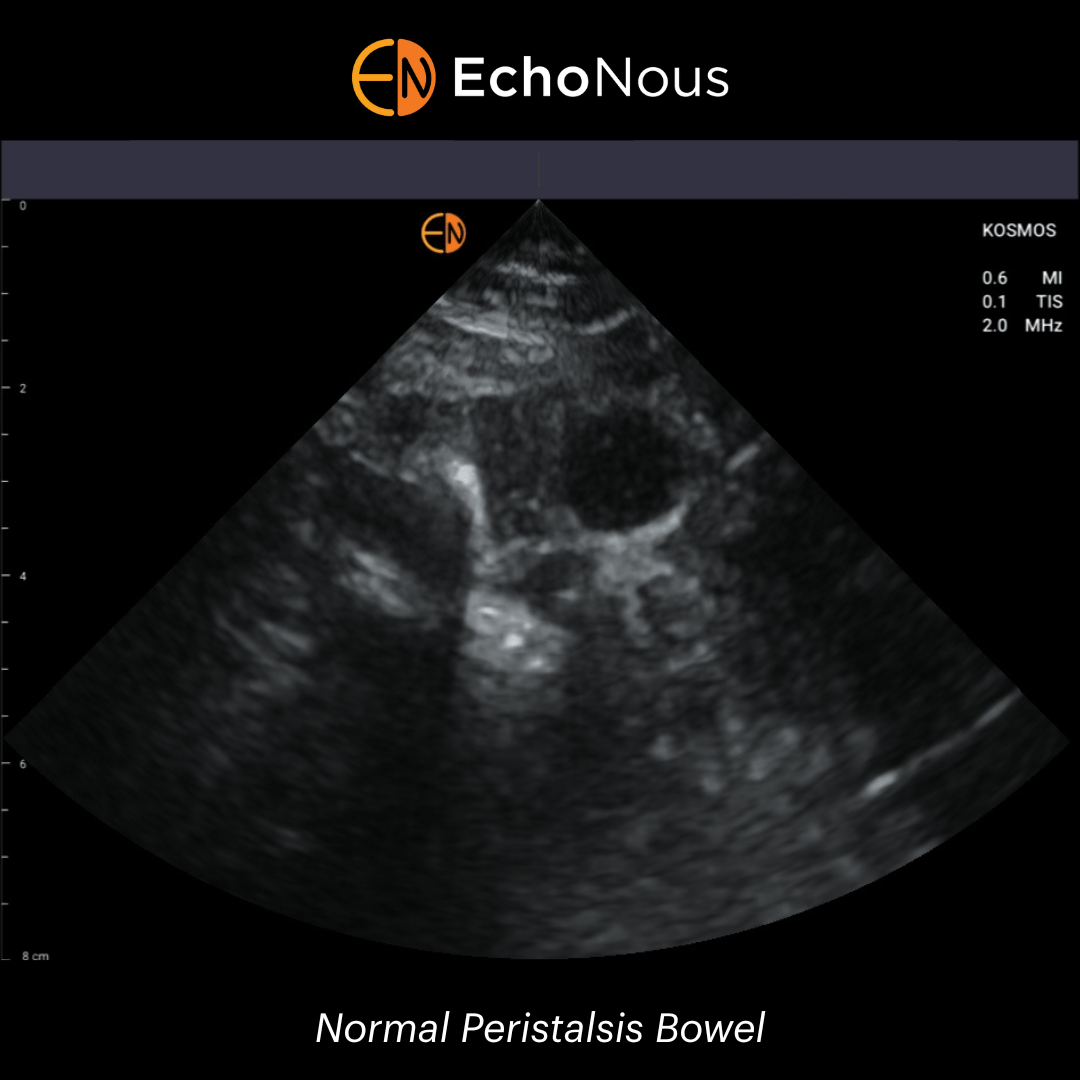
Liliana Aguilar, MD: Yes, I have a certificate in ultrasound, allowing me to perform various types of ultrasounds. This includes abdominal ultrasounds, which have been beneficial in detecting issues like gallbladder problems and irritable colon, and we have used them to rule out appendicitis. We’ve even used it for breast abscesses and identified fetal positions. This training and certification are crucial in handling ultrasound equipment, ensuring accurate diagnoses, and timely patient care.
POCUS and Telemedicine in Emergent Care
Luke Baldwin: Excellent. That’s amazing. Can you share any impactful cases?
Liliana Aguilar, MD: Certainly, one memorable case involved a 12-13-year-old girl with a noticeably swollen abdomen. Her mother brought her in, concerned she might be pregnant. After an examination, it was evident she wasn’t carrying a baby. Gynecology and Pediatrics evaluated her, revealing a tubulation in the ovary. The child was then referred to the children’s hospital.
We conducted the ultrasound here during the patient’s examination. The situation was severe, and the girl underwent surgery at the hospital. Thankfully, she’s now here, and her life was saved. She even came by to express gratitude for the support, and all the services were provided free of charge. She’s in her third year of high school, and it has impacted the family so much that her mother has come in and thanked us in tears.
It was shocking because no one, not even the mother, anticipated the issue. The abdomen grew little by little, leading us to believe it was a growing baby. However, it turned out to be an ovarian tumor, fortunately ruled out as malignant. The concern was real, fearing the girl might lose her life, but she underwent treatment, had surgery while still in her normal school year, and her life was saved.
Luke Baldwin: Can you tell me how the ultrasound system works with telemedicine? In which cases do you use it with a patient? Do you use it yourself to find out what is happening, or do you always use it in consultation with a specialist?
Liliana Aguilar, MD: The example I shared is a real-life scenario demonstrating our equipment’s practical utility. In emergencies, especially during the early morning hours, when a pregnant woman or another patient presents with severe pain, I use the equipment to track the patient and facilitate necessary referrals. Our gynecologist is available around the clock, making it easier for us to collaborate.
We rely on the equipment throughout the day—morning, afternoon, and night—for emergencies and routine cases. Since the ultrasound is equipped with Bluetooth connectivity, it allows the gynecologist to observe and guide me remotely, expediting diagnosis and treatment. We organize patient care based on pathology, utilizing gynecology, internal medicine, pediatrics, and general surgery services.
The equipment has proven invaluable, particularly in cases involving pregnant women. Whether I’m directly involved in patient care or collaborating with the gynecologist, the equipment ensures seamless communication and swift decision-making. This has been crucial in saving limbs for diabetic patients dealing with foot issues. By involving the surgeon and internist, we monitor and assist in wound healing, preventing the need for amputation.
Telemedicine, coupled with the support of our pediatrician, has been vital, especially in urgent situations. The equipment serves us well as a versatile tool, providing timely support across medical disciplines.
Real World POCUS Applications
Luke Baldwin: Wow, that’s amazing. Could you paint a picture of the before and after? What can you do now that you couldn’t do in the past?
Liliana Aguilar, MD: Now, we can avoid unnecessary transfers, especially for patients in remote areas with limited economic resources. In the past, important transfers lacked timely attention. With our equipment, we address these situations locally whenever possible. For diabetic patients in rural areas without access to glucose measurement tools, support is crucial.
Ultrasound allows us to identify emergencies in real time—a capability we lacked as a first-level health service without ultrasound equipment. Thanks to the support of 19Labs and the telemedicine program, we can now provide these essential services to benefit our patients. The addition of high-speed internet further streamlines our processes, allowing faster reporting, immediate communication with superiors during emergencies, and seamless connections with the hospital. It’s a significant advantage.
Beyond its ultrasound applications, telemedicine serves as a lifeline for people with diabetes in remote areas where monitoring glucose readings is challenging. This telemedicine kit facilitates continuous monitoring, timely treatment, and assessment of emergency levels, preventing issues from escalating into emergencies.
The issue often lies in the fingers, as ulcers sometimes do not heal. Yet, involving the surgeon and the internist allows close monitoring, assisting in wound healing, and eliminating the need for amputation through general surgery, as mentioned earlier. This is crucial, particularly in emergencies when quick decisions are required.
Additionally, we use the telemedicine kit ourselves to troubleshoot problems. This proactive approach, especially with diabetic patients in collaboration with internal medicine, has effectively prevented amputations. It’s about identifying issues early before they become severe, and this comprehensive approach has significantly impacted our clinic’s capabilities in the medical world. It empowers us to file reports, engage in specialist consultations, and enhance our clinic’s reach and effectiveness.
Maria del Carmen Ortegon, 19Labs, Latin America Operations: We’ve received feedback from many other regional clinics that they love the Kosmos because of its small size and beautiful resolution. It is so much clearer than any other solution that they’ve been able to have. They had not previously heard of it, and they’ve just loved it.
Cardiac Imaging and AI in Rural Healthcare
Luke Baldwin: Are there any current or potential uses for cardiac imaging, especially ultrasound technology, in detecting heart failure or cardiovascular disease? I am curious about the potential benefits of using AI-powered solutions to address your community’s needs, especially in detecting cardiovascular diseases.
Liliana Aguilar, MD: Absolutely. A heart ultrasound would be incredibly beneficial, especially in identifying issues like insufficiency. This could aid in understanding cardiovascular conditions and improving patient care. The community has shown great interest in the capabilities of ultrasound, and there’s potential for even broader applications in the future.
Luke Baldwin: What do you envision for the future of this technology? What developments are on the horizon?
Liliana Aguilar, MD: I see the potential for a broader application in various medical fields if more options become available to us. The versatility of ultrasound opens up possibilities for diverse uses. We have Kosmos with AI for the heart and abdomen, and I find its capabilities quite impressive.
The technology has already demonstrated its value, and as it becomes more accessible, we can continue addressing various health issues locally. The prospect of additional training and applications, alongside advancements in telemedicine, could significantly enhance healthcare delivery in our community.
Luke Baldwin: Muchas gracias, Dr. Aguilar!. I truly appreciate your time and insights during this conversation. It’s incredibly helpful for us and I’m sure many others who read this. We’d love to stay connected and assist in any way we can.
Liliana Aguilar, MD: We genuinely appreciate your time and dedication to collaborating with us in advancing healthcare technology. Thank you for your support.
To learn more about Kosmos, contact us today!