The Magic Formula for Supporting Nurses: A New Perspective on Ultrasound-Guided Procedures
What is POCUS in Nursing?
Nursing management faces the critical challenge of combating burnout among staff, which affects retention, job satisfaction, and patient care quality. High workloads and stressful procedures like difficult vascular access can contribute to this widespread issue.
Integrating point-of-care ultrasound (POCUS) into everyday practice offers a solution by streamlining workflows, improving success rates in IV insertions, and freeing up nurses for more meaningful patient interactions. This article describes how ultrasound – supported by targeted POCUS education – empowers nursing teams, improves operational efficiency, and enhances overall patient care.
Key Takeaways:
- Burnout among nurses is a growing problem
- Integrating point of care ultrasound (POCUS) could be a viable solution to ameliorating burnout among nursing staff
- Ultrasound guided procedures significantly reduce the time it takes to gain IV access
- By learning POCUS techniques, nurses can increase quality time spent with patients and potentially reduce costs and rates of burnout
Table of contents
- The Magic Formula for Supporting Nurses: A New Perspective on Ultrasound-Guided Procedures
- What is POCUS in Nursing?
- The Challenge of Burnout in Nursing
- The Impact of Ultrasound-Guided Procedures on Workflow and Alleviating Burnout
- Evidence of Improved Success Rates
- Connection to Burnout Reduction
- Empowering Nurses with Technology: The Case of EchoNous
- Time Savings and Efficiency
- Quality Time with Patients: Enhancing Patient Satisfaction and Nurse Engagement
- Impact on Patient Satisfaction and Outcomes
- Cost Savings and Economic Implications
- Evidence of Cost Effectiveness
- Conclusion
The Challenge of Burnout in Nursing
Burnout is a persistent issue in nursing, with more than 60% of nurses experiencing its effects [1]. For nursing management, this translates into high turnover rates, increased recruitment costs, and the need for constant retraining, all of which impact the bottom line and patient care quality.
Tasks such as vascular access, which can be routine yet challenging, are significant contributors to nurse stress [2]. Management can address these challenges by adopting technologies that streamline these processes, such as ultrasound-guided IV insertion using POCUS.

The Impact of Ultrasound-Guided Procedures on Workflow and Alleviating Burnout
POCUS, particularly for vascular access, offers a high-impact intervention to reduce nurse workload and improve procedural success rates. The ability to see veins in real time reduces the number of attempts required for successful IV insertions, minimizing patient discomfort and procedural time.
This efficiency not only enhances patient satisfaction but also significantly reduces the stress on nurses, allowing them to focus on higher-priority patient care tasks like patient handoffs, charting, and filling orders.
Evidence of Improved Success Rates
In a systematic review, it was concluded that “Ultrasound-guided peripheral cannulation achieves a higher success rate, a reduction in the overall procedure time, and fewer total attempts when compared to the conventional palpation technique demonstrating greater efficacy in peripheral venous access” [3].
Another study by Tran, Q. K. et al. (2021) concluded that ultrasound-guided venous cannulation is advantageous over landmark-based cannulation methods for the first successful placement of cannulation [4].
The increased efficiency helps streamline operations, reducing time spent on repeated attempts and allowing nurses to manage more patients effectively, directly addressing burnout.
Connection to Burnout Reduction
Although direct links between POCUS and reduced burnout are still emerging, studies indicate that streamlined workflows and reduced procedural stress correlate with lower burnout levels.
The integration of POCUS and targeted POCUS education reduces routine task burdens, empowering nurses with the skills to perform procedures with more confidence and less reliance on physicians, which ultimately enhances job satisfaction.

Ready to empower your nursing team? Discover how EchoNous can enhance your facility’s efficiency with affordable, user-friendly POCUS technology for vascular access.
Empowering Nurses with Technology: The Case of EchoNous
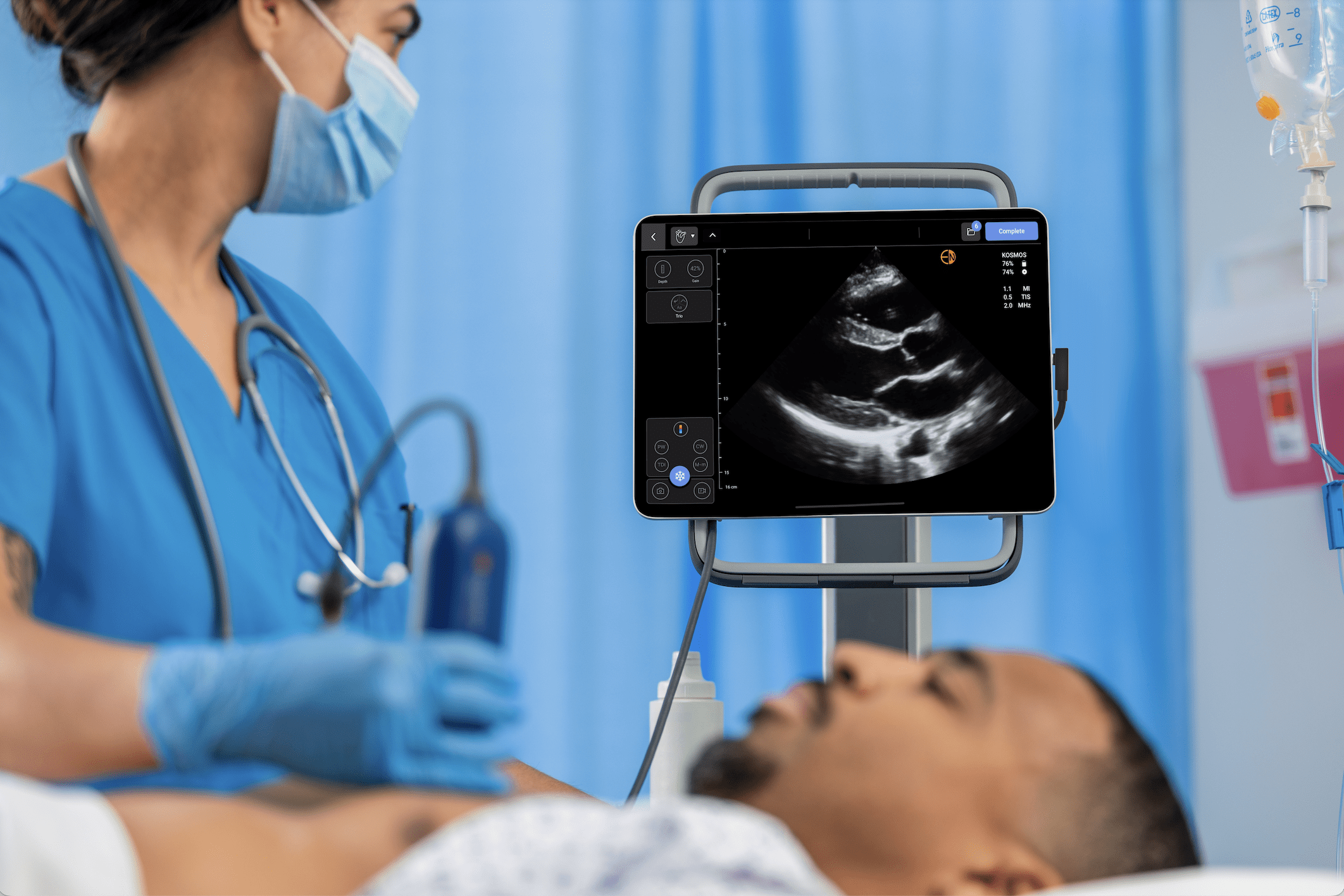
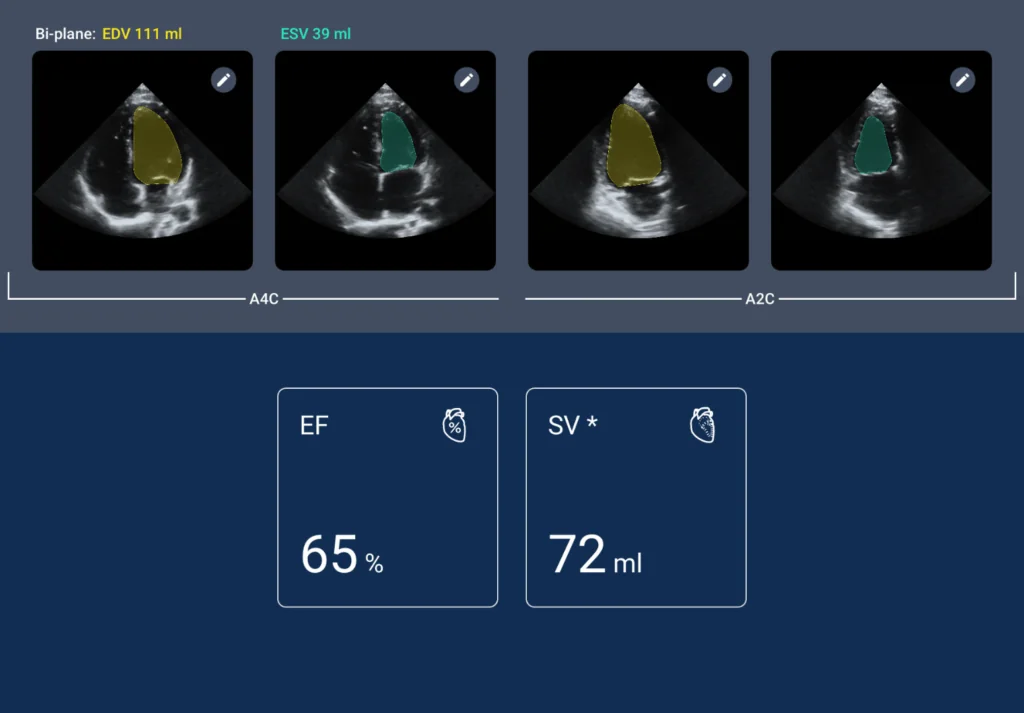
The Kosmos ultrasound system by EchoNous provides a user-friendly interface that reduces the learning curve from weeks to just hours, making it accessible even for those new to point-of-care ultrasound (POCUS). For nursing management, this means less time spent on training and more time deploying skilled staff where they are most needed.
Kosmos’ intuitive design empowers nurses to perform ultrasound-guided procedures quickly and confidently, enhancing the overall efficiency of nursing teams. Studies have shown that simple teaching interventions can enable novices to competently perform ultrasound-guided peripheral IV insertions, leading to significant positive outcomes for patients and healthcare systems [5].
Time Savings and Efficiency
EchoNous’ POCUS technology can significantly reduce the time required for IV insertions. The Kosmos system’s intuitive design and real-time imaging capabilities enable quick, accurate assessments of vascular structures, allowing nurses to make immediate decisions and perform insertions with confidence.
This rapid workflow enhancement translates into time savings that can be reallocated to patient care, charting, or other critical tasks, ultimately reducing the cognitive load on nurses.
Quality Time with Patients: Enhancing Patient Satisfaction and Nurse Engagement
One of the most significant benefits of adopting ultrasound-guided procedures is the potential to free up time for nurses, allowing them to engage more deeply with their patients. Quality time with patients is not just a necessity; it is essential for patient satisfaction and nursing job satisfaction.
Studies have shown that increased patient-nurse interaction leads to better patient outcomes, higher satisfaction scores, and a stronger sense of accomplishment for healthcare providers [6,7].
Impact on Patient Satisfaction and Outcomes
Ultrasound-guided vascular access not only improves the technical success of procedures but also enhances the overall patient experience. Studies have found that patients who underwent ultrasound-guided IV insertions reported significantly higher satisfaction scores than those who received traditional blind insertions [8,9].
The reduced pain, fewer attempts, and quicker procedure times contributed to a more positive perception of care, which in turn reflects positively on the healthcare facility.
Cost Savings and Economic Implications
Beyond the clinical benefits, ultrasound-guided procedures can also offer economic advantages by reducing the costs associated with failed insertions, complications, and extended hospital stays.
Inserting an IV successfully on the first attempt avoids additional supplies, personnel time, and potential treatments for complications such as infections or thrombosis. The improved efficiency and reduced resource utilization align with broader healthcare goals of cost containment and resource optimization 10,11].
Evidence of Cost Effectiveness
Research has indicated that savings in operational costs quickly offset the initial investment in ultrasound technology. Multiple studies have estimated that ultrasound-guided IV insertions saved hospitals’ average cost per procedure due to reduced complications and resource use. These cost-saving aspects add another layer of appeal for healthcare systems aiming to improve both patient care and financial performance [10-12].
Studies have estimated that using ultrasound guidance for central venous cannulation is cost-effective, with economic evaluations showing that the marginal cost per procedure is less than $10 when used for 15 procedures per week, resulting in $2000 worth of savings and 90 complications avoided per 1000 procedures.
The findings suggest that ultrasound guidance, compared to traditional methods, not only enhances efficiency and reduces complications but also offers substantial resource savings, making it a valuable first-line strategy for improving patient care in populations with difficult vascular access (DVA) [10-12].
Conclusion
The integration of ultrasound-guided procedures into nursing practice represents a significant step forward in addressing one of the profession’s most pervasive challenges: burnout.
By enhancing efficiency, reducing stress, and empowering nurses with cutting-edge technology like the Kosmos ultrasound system, healthcare facilities can foster a more supportive environment where nurses feel valued and capable.
This, in turn, enhances patient care, boosts satisfaction, and contributes to a more sustainable nursing workforce. As healthcare continues to evolve, the adoption of innovative tools and techniques will be critical in ensuring that nurses remain at the forefront of patient-centered care.
Enhance your nursing expertise with the cutting-edge Kosmos system for vascular access. Benefit from improved patient satisfaction, procedural safety, and continuous scanning capability. Embrace the mobility and ease of cleaning designed for the rigorous demands of hospital use. Plus, we offer flexible payment options and a robust 5-year warranty.
Elevate your vascular access first stick success rate – schedule your Kosmos demo today and see the difference precise imaging can make in your practice

Contributing Author: Dr. Abhishek Gupta, BDS, MDS
Medical Reviewer: Dr. Danielle Kelvas, MD
References
- Nurse Burnout. (2024, February 1). What is it and How to prevent it. ANA Nursing Resource Hub.
- Jackson Andrew. (2003). Reflecting on the nursing contribution to vascular access. British Journal of Nursing. 12 (11):657-65.
- Ye, X., & Li, M. (2022). Comparison of Ultrasound Guided and Conventional Techniques for Peripheral Venous Catheter Insertion in Pediatric Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Frontiers in Pediatrics, 9, 797705.
- Tran, Q. K., Flanagan, K., Fairchild, M., Yardi, I., & Pourmand, A. (2022). Nurses and Efficacy of Ultrasound-Guided Versus Traditional Venous Access: A Systemic Review and Meta-Analysis. Journal of Emergency Nursing, 48(2), 145-158.e1.
- Hoskins, M. J., Nolan, B. C., Evans, K. L., & Phillips, B. (2023). Educating health professionals in ultrasound guided peripheral intravenous cannulation: A systematic review of teaching methods, competence assessment, and patient outcomes. Medicine, 102(16), e33624.
- Vujanić, J., Mikšić, Š., Barać, I., Včev, A., & Lovrić, R. (2022). Patients’ and Nurses’ Perceptions of Importance of Caring Nurse–Patient Interactions: Do They Differ? Healthcare, 10(3), 554.
- Gabay, G. (2023, March 06). Nurse-patient interactions in intensive care, transitions along the continuum of hope, and post-discharge management of chronic illness—A mixed methods narrative inquiry. Frontiers in Public Health, 11.
- Malik, A., Dewald, O., Gallien, J., Favot, M., Kasten, A., Reed, B., Wells, R., & Ehrman, R. R. (2023). Outcomes of Ultrasound Guided Peripheral Intravenous Catheters Placed in the Emergency Department and Factors Associated with Survival. Open Access Emergency Medicine : OAEM, 15, 177–187.
- Schoenfeld, E., Shokoohi, H., & Boniface, K. (2011). Ultrasound-Guided Peripheral Intravenous Access in the Emergency Department: Patient-Centered Survey. Western Journal of Emergency Medicine, 12(4), 475–477.
- Bahl, A., Johnson, S., Hijazi, M., Mielke, N., & Chen, N.-W. (2024). Cost effectiveness of ultrasound-guided long peripheral catheters in difficult vascular access patients. The Journal of Vascular Access, 25(4), 1204–1211.
- Ablordeppey, E. A., Koenig, A. M., Barker, A. R., Hernandez, E. E., Simkovich, S. M., Krings, J. G., Brown, D. S., & Griffey, R. T. (2022). Economic Evaluation of Ultrasound-guided Central Venous Catheter Confirmation vs Chest Radiography in Critically Ill Patients: A Labor Cost Model. Western Journal of Emergency Medicine, 23(5), 760–768.
- Calvert, N., Hind, D., McWilliams, R., Davidson, A., Beverley, C., & Thomas, S. (2004). Ultrasound for central venous cannulation: Economic evaluation of cost-effectiveness. Anaesthesia, 59, 1116–1120.